Discovering what causes arthritis in the shoulder can be key to better management. Whether it’s the natural wear and tear as years go by, the immune system attacking joint tissue, or lingering effects from an old injury, these are the primary forces at play. In the following sections, learn how these factors contribute to your shoulder pain and what strategies can help alleviate it.
Key Takeaways
- Shoulder arthritis is predominantly caused by two types: Degenerative Joint Disease (osteoarthritis) due to cartilage deterioration, and Inflammatory Arthritis (such as rheumatoid arthritis) caused by the immune system attacking joint tissues.
- Symptoms of shoulder arthritis include persistent pain, stiffness, reduced range of motion, and sensations such as grinding or cracking; the condition can significantly impair daily activities and varies depending on which part of the shoulder is affected.
- Treatment options for shoulder arthritis range from non-surgical interventions like physical therapy and medications to surgical procedures such as arthroscopic debridement or shoulder replacement, depending on the severity of the condition.
Understanding Shoulder Arthritis
Our mobility and strength hinge on the complex structure of the shoulder joint, also known as the shoulder socket. It’s composed of the humerus (upper arm bone) and the scapula (shoulder blade), working cohesively to provide us with a remarkable range of motion. The stability and mobility of the shoulder are further enhanced by the glenohumeral capsule, labrum, and ligaments, which offer additional support. However, when damage occurs to the cartilage inside the shoulder joint, we find ourselves grappling with shoulder arthritis.
In the realm of shoulder arthritis, two forms take the lead: Degenerative Joint Disease and Inflammatory Arthritis. Both types can profoundly impact the quality of life, resulting in pain and limiting mobility. Gaining knowledge about these forms of arthritis allows us to manage the condition proactively and safeguard our shoulder health.
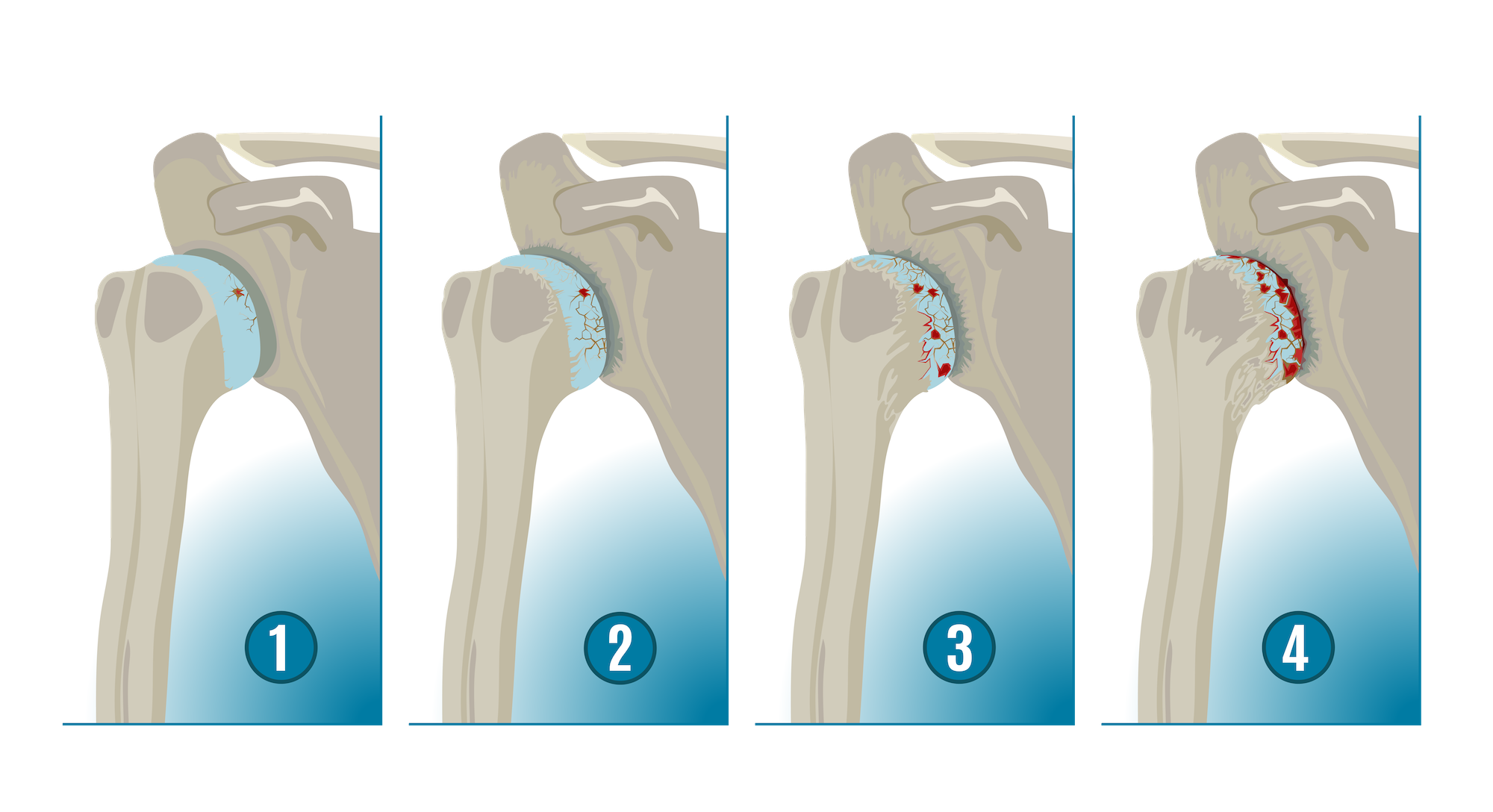
Degenerative Joint Disease
Also known as osteoarthritis, Degenerative Joint Disease is a common form of shoulder arthritis. It is characterized by the gradual deterioration of cartilage, starting with softening, leading to surface cracking, and ultimately resulting in complete wearing away. This exposes the underlying bone and results in pain and inflammation.
The progression of the disease causes the bones to rub together, leading to the formation of bone spurs, which further intensify the discomfort.
Inflammatory Arthritis
In contrast to osteoarthritis, Inflammatory Arthritis, such as rheumatoid arthritis, is an autoimmune disorder. In this case, the body’s immune system mistakenly attacks healthy joint tissues, leading to inflammation and damage in the shoulder joint lining. Interestingly, rheumatoid arthritis affects both shoulder joints equally, unlike other forms of arthritis which may favor one joint over the other.
Conditions like post-traumatic injuries and rotator cuff tear arthropathy can also contribute to shoulder arthritis.
Recognizing Symptoms of Shoulder Arthritis
Identifying shoulder arthritis symptoms paves the way for seeking appropriate treatment. The most common symptoms include mild-to-severe pain, stiffness, and loss of range of motion. Activities such as reaching overhead, heavy lifting, and engaging in sports can cause discomfort for individuals with shoulder arthritis. As the disease progresses, even everyday tasks such as bathing, grooming, writing, and using the computer may cause pain. In some cases, the pain can radiate from the shoulder down to the arm, elbow, and wrist.
Depending on the specific joints affected, the symptoms of shoulder arthritis may vary. The glenohumeral joint and rotator cuff involvement can result in a deep ache on the side of the shoulder, while arthritis in the AC joint can cause discomfort that interferes with sleep, especially when lying on the affected side.
Additionally, individuals may experience the following symptoms in the shoulder joint:
- Grinding
- Clicking
- Cracking
- Sensations of locking or sliding
These unique symptoms often arise as the joint experiences increased friction due to the wear and tear of cartilage.
Glenohumeral Joint and Rotator Cuff Involvement
When arthritis affects the glenohumeral joint, discomfort and a deep ache are often localized on the side of the shoulder. The rubbing together of the bones due to arthritic damage to the glenohumeral joint’s cartilage leads to inflammation and pain.
Additionally, shoulder arthritis can develop as a result of a condition known as rotator cuff tear arthropathy, which occurs after a massive and prolonged tear in the rotator cuff.
AC Joint Symptoms
AC joint arthritis is another specific form of the condition. It occurs when the junction where the clavicle meets the highest point of the shoulder blade undergoes deterioration and inflammation. The symptoms are characterized by pain at the top of the shoulder and sometimes extending to the side of the neck.
Identifying Causes and Risk Factors
Effectively managing shoulder arthritis requires a thorough understanding of its causes and risk factors. Various forms of shoulder arthritis such as:
- Osteoarthritis
- Rheumatoid arthritis
- Post-traumatic arthritis
- Rotator cuff tear arthropathy
- Avascular necrosis
originate from different causes.
The most prevalent form, osteoarthritis, often results from the age-related deterioration and gradual wear and tear of the cartilage in the shoulder joint. Repetitive physical tasks and sports involving substantial shoulder movement can accelerate the development of osteoarthritis. Interestingly, females are found to have a higher likelihood of developing shoulder osteoarthritis than males.
Age-Related Wear and Tear
Osteoarthritis development is significantly influenced by age. This form of arthritis typically affects older individuals and becomes more prevalent as people age. It is most common in people over the age of 50, with the risk increasing with each passing year.
This is due to the wear and tear that comes with aging, also known as Degenerative Joint Disease.
Autoimmune Diseases
Shoulder arthritis can also stem from autoimmune diseases like rheumatoid arthritis. Rheumatoid arthritis is an inflammatory autoimmune condition where the immune system mistakenly attacks the lining of the joint. Unlike other forms of arthritis, rheumatoid arthritis can affect both shoulders simultaneously, indicating that autoimmune diseases can have symmetrical manifestations in the body.
Previous Shoulder Trauma
Arthritis of the shoulder, can also arise from previous shoulder trauma. Post-traumatic arthritis develops after an injury to the shoulder. Shoulder injuries such as fractures or dislocations can precipitate the onset of post-traumatic arthritis.
Additionally, a significant rotator cuff tear, known as rotator cuff tear arthropathy, can lead to arthritis as the humeral head rubs against other bones.
Diagnosing Shoulder Arthritis
A comprehensive shoulder arthritis diagnosis process commences with a detailed account of the patient’s symptoms and a thorough physical examination, which includes evaluating the range of motion and strength in the shoulder. In addition, doctors utilize various imaging techniques such as X-rays, CT scans, and MRI scans to diagnose shoulder arthritis and assess its severity.
In some cases, an injection of local anesthetic may be administered into the shoulder joint to provide temporary pain relief and serve as a supporting diagnostic tool for arthritis.
Evaluating Range of Motion and Strength
When diagnosing shoulder arthritis, assessing the range of motion is a critical part of the physical examination. It aids in identifying limitations and pain. Orthopedic surgeons often use tools such as a goniometer, which measures angles in degrees, and inclinometers, especially used for spinal angles, to evaluate joint range of motion.
The testing may involve passive motion by a therapist, active motion by the patient, or active-assistive motion involving devices or therapist assistance.
Imaging Techniques
Imaging techniques play an essential role in diagnosing shoulder arthritis. High-resolution imaging such as ultrasound and MRI provide detailed visualizations of the joint. These scans offer superior soft tissue contrast, facilitating the differentiation of structures within the shoulder joint and helping doctors assess the severity of arthritis.
Non-Surgical Treatment Options
Non-surgical treatments typically form the first line of defense when shoulder arthritis symptoms initially surface. These treatments include physical therapy, medications, and lifestyle modifications. Heat treatment can be beneficial before performing exercises to warm up the shoulder joint.
Medications such as acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) are often used to manage pain and inflammation. In addition, avoiding activities that exacerbate shoulder pain and applying ice for pain relief are recommended lifestyle modifications.
Physical Therapy and Exercises
Managing shoulder arthritis non-surgically heavily relies on physical therapy. It begins shortly after surgery with gentle exercises aimed at reducing pain and enhancing the range of motion. Strengthening exercises for the shoulder typically begin three months after surgery to ensure proper healing and mobility of the joint.
The therapy involves range of motion testing conducted initially, midway, and at the end of the program to establish a baseline, assess progress, and evaluate permanent improvement or residual impairment. Daily stretching, specifically for two to three minutes, is essential in maintaining shoulder mobility and in the prevention of further loss of motion due to arthritis.
Medications and Supplements
In addition to physical therapy, medications and supplements are vital in managing the symptoms of shoulder arthritis. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) and acetaminophen are commonly employed to manage shoulder arthritis pain, but the dosing should always be discussed with a physician.
To provide immediate pain relief, corticosteroid injections typically include a numbing agent. Synthetically manufactured hyaluronic acid injections can relieve shoulder arthritis pain for up to two years.
Surgical Interventions for Shoulder Arthritis
Surgical intervention becomes necessary when non-surgical treatments fail to provide adequate relief. Arthroscopic shoulder debridement and shoulder replacement surgery are the two main surgical procedures for treating shoulder arthritis. Shoulder replacement is the preferred surgical procedure for advanced arthritis, such as bone-on-bone conditions in the glenohumeral joint.
The choice of surgical procedure, including the type of shoulder replacement, depends on several factors including the patient’s age, the extent of arthritis, and the condition of the rotator cuff tendons.
Arthroscopic Shoulder Debridement
Arthroscopic shoulder debridement is used to remove loose fragments of cartilage and bone in the joint in cases of early shoulder arthritis. The success of the procedure is measured by the relief of pain for 12 to 24 months, although it’s not a permanent solution to arthritis.
The procedure utilizes an arthroscope, a small camera, to navigate tiny surgical instruments during microsurgery. The surgery can last from one to two hours, depending on the extent of tendon damage.
Shoulder Replacement Surgery
In cases of advanced arthritis, shoulder replacement surgery is often the recommended treatment. In an anatomic total shoulder replacement, the ball and socket parts of the shoulder joint are replaced with artificial components. This procedure aims to alleviate pain and restore function in the shoulder. Reverse total shoulder replacement is mainly utilized when a patient has arthritis in the shoulder coupled with a rotator cuff tear.
After shoulder replacement surgery, a shoulder sling is used to protect the replacement and, in the case of an anatomic shoulder replacement, to support the rotator cuff repair. Formal physical therapy typically begins one to two weeks after an anatomic shoulder replacement to aid in recovery.
Post-Surgery Rehabilitation and Recovery
To restore function and relieve pain, it’s crucial to properly navigate the post-surgery recovery process. Following shoulder surgery, patients can expect:
- A period of pain and sleep disruption for the first 4-6 weeks
- Immobilization in a sling during this time
- Physical therapy beginning shortly after surgery with gentle exercises aimed at reducing pain and enhancing range of motion
While the general recovery process after shoulder surgery requires about six months, patients can anticipate continued improvement for up to a year following the procedure.
Recovery Timeline
For patients who have undergone surgery for shoulder arthritis, it’s important to comprehend the recovery timeline. After surgery, patients receive specific instructions for:
- wound care
- bandaging
- managing pain
- mobility restrictions
A sling is commonly used for immobilization to provide stability to the shoulder after surgery, with an average necessity period of 4-6 weeks.
Rehabilitation and physical therapy are crucial to improve or maintain range of motion and to help increase strength post-surgery.
Post-Operative Care and Follow-Up
Optimal recovery relies heavily on adherence to post-operative care guidelines and attendance at follow-up appointments. Stitches from shoulder surgery are removed at the first follow-up appointment, which is usually one to two weeks after the surgery. Patients must immediately contact their surgeon if they experience any of the following symptoms:
- Swelling at the incision site
- Drainage from the incision site
- Redness or pain at the incision site
- Fever over 101 degrees F
Pain medications are prescribed to manage discomfort after shoulder surgery.
Summary
In conclusion, shoulder arthritis is a prevalent condition that can significantly impact the quality of life. Its symptoms include pain, stiffness, and a loss of range of motion, and it is often caused by age-related wear and tear, autoimmune diseases, or previous shoulder trauma. While non-surgical treatments such as physical therapy and medications can provide relief, surgical interventions may be necessary in severe cases. Post-operative care and rehabilitation are crucial for recovery and the restoration of shoulder function. Armed with this knowledge, you can better understand and manage shoulder arthritis, improving your quality of life.
Frequently Asked Questions
What is the main cause of shoulder arthritis?
The main cause of shoulder arthritis is age-related wear and tear on the shoulder joint, leading to osteoarthritis, but it can also be caused by autoimmune diseases like rheumatoid arthritis or previous shoulder trauma.
What are the symptoms of shoulder arthritis?
Shoulder arthritis symptoms include mild-to-severe pain, stiffness, and loss of range of motion in the shoulder. Pain may also radiate down the arm, elbow, and wrist.
How is shoulder arthritis diagnosed?
Shoulder arthritis is diagnosed through a physical examination, detailed medical history, and imaging techniques like X-rays, CT scans, and MRI scans. These methods help to accurately identify the condition and develop a suitable treatment plan.
What are the non-surgical treatment options for shoulder arthritis?
Non-surgical treatment options for shoulder arthritis include physical therapy, pain and anti-inflammatory medications, PRP, and lifestyle modifications such as avoiding activities that exacerbate shoulder pain. These options can help manage symptoms and improve shoulder function.