Frozen shoulder, occurs when the connective tissue around the shoulder joint becomes inflamed and tightened, limiting movement. Common contributing factors include prolonged immobility, certain medical conditions like diabetes, and age-related hormonal changes. In this post, we’ll explore these causes in-depth, alongside symptoms and effective treatments.
Key Takeaways
- Frozen shoulder is characterized by painful stiffness and reduced mobility due to the thickening and tightening of the shoulder capsule, often triggered by immobility or medical conditions.
- Risk factors include age (typically between 40 and 60), gender (more common in women), and certain medical conditions like diabetes and thyroid disorders.
- Effective treatment often involves a combination of nonsurgical options like physical therapy and anti-inflammatory medications, with surgery considered when these approaches fail to relieve symptoms.
Understanding Frozen Shoulder
Frozen shoulder, or adhesive capsulitis, is a painful and limiting condition marked by a progressive loss of shoulder motion and increasing stiffness. As the condition advances, both active and passive range of motion become restricted, making it challenging to perform everyday tasks.
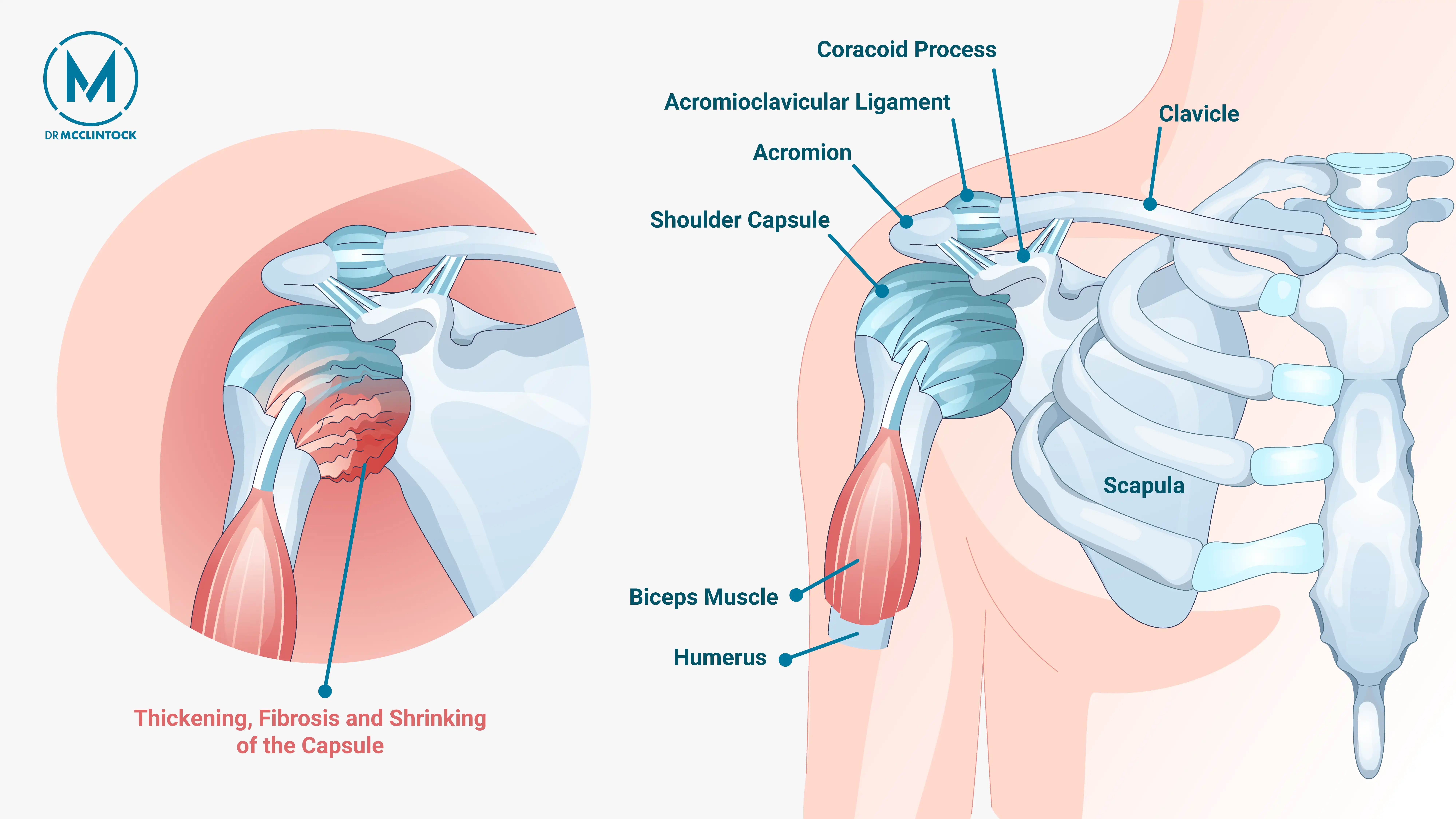
The condition develops when the connective tissue surrounding the shoulder joint, known as the shoulder capsule, becomes inflamed. This inflammation leads to the formation of scar tissue, which restricts shoulder movement and increases shoulder stiffness. A reduction in synovial fluid within the joint worsens the stiffness and discomfort.
Unlike a rotator cuff tear, which may still allow some degree of motion, frozen shoulder typically causes severe immobility. Early diagnosis and appropriate intervention are essential for restoring movement and reducing pain.
Causes and Risk Factors for Frozen Shoulder
The exact cause of frozen shoulder is not always clear, but certain factors are known to contribute to its onset. One of the most common contributing factors is prolonged immobility of the arm, such as following a surgery or fracture. When the shoulder is immobilized for extended periods of time, the joint capsule can stiffen and tighten, increasing the risk of adhesive capsulitis.
In addition, certain medical conditions and demographic factors increase the likelihood of developing frozen shoulder. In the following subsections, we’ll explore these factors.
Medical Conditions
Certain medical conditions can significantly increase the risk of developing frozen shoulder. Individuals with diabetes, for example, are at a heightened risk, and those with long-standing diabetes may experience more severe cases and slower recovery.
Other conditions, including cardiovascular disease, Parkinson’s disease, and thyroid disorders, are also associated with a higher risk.
Demographic Factors
Frozen shoulder most commonly affects individuals aged 40 to 60 and is more frequently diagnosed in women. While this condition may still occur outside of these demographics, trends suggest that hormonal and age-related changes may influence susceptibility.
Symptoms of Frozen Shoulder
Frozen shoulder symptoms typically progress through three stages:
- Freezing stage (lasts around 2 to 9 months): Pain gradually increases and shoulder movement becomes increasingly restricted.
- Frozen stage (4 to 12 months): Pain may lessen slightly, but stiffness becomes more severe, further limiting shoulder function.
- Thawing stage (5 to 24 months): Mobility slowly improves, and pain continues to decrease as the shoulder “thaws.”
Another possible symptom of frozen shoulder is a significant loss of external rotation. Internal rotation may also be limited.
Recognition of frozen shoulder symptoms is important for starting effective treatment early and improving long-term outcomes.
Diagnosing Frozen Shoulder
Diagnosing frozen shoulder involves a combination of clinical evaluation, including a medical history review and physical exam, along with imaging tests. This comprehensive approach helps to rule out other shoulder conditions and confirm an accurate diagnosis.
Clinical Evaluation
Clinical evaluation, including a thorough discussion of the main symptoms and medical history, is the primary method to diagnose frozen shoulder. This will include a discussion of pain levels and mobility limitations, as well as how these affect daily activities.
A physical examination will be conducted to assess reductions in shoulder mobility, especially in movements like flexion, abduction, and rotations. Your doctor will evaluate your range of motion and assess your pain levels during movement.
Imaging Tests
Imaging tests play a supportive role in the diagnosis of frozen shoulder. They are generally used to exclude other shoulder conditions such as arthritis, fractures, or rotator cuff tears.
Shoulder X-rays help by ruling out bony abnormalities and signs indicative of arthritis. Magnetic resonance imaging (MRI) offers detailed imaging of soft tissues, which can confirm or rule out other shoulder conditions.
Treatment Options for Frozen Shoulder
Treatment options for frozen shoulder include a combination of nonsurgical and surgical interventions, depending on the severity of the condition. Many patients improve significantly with conservative approaches, and surgery is considered when symptoms persist despite nonsurgical treatment.
Nonsurgical Treatments
Nonsurgical care is the first-line approach. Key treatments include:
- Physical therapy, guided by an experienced therapist, aims to improve shoulder flexibility and function through specific exercises.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce pain and swelling.
- Corticosteroid injections, delivered directly into the shoulder joint, can provide powerful anti-inflammatory effects and reduce pain and mobility.
- Platelet-Rich Plasma (PRP) injections, which involves injecting a concentration of the patient’s own platelets into the shoulder joint, may help reduce inflammation and promote healing. While still considered an emerging treatment, PRP is sometimes used alongside physical therapy when standard options have limited effect.
During recovery, patients are generally encouraged to gradually increase activity while protecting the joint.
Surgical Interventions
When nonsurgical treatment fails to provide adequate relief, surgical interventions may be considered. Two common options are shoulder manipulation and arthroscopic surgery. An experienced orthopedic surgeon can help recommend the best course of action depending on your overall health status and recovery goals.
Shoulder manipulation under anesthesia can loosen the tight joint capsule without the need for incisions. Arthroscopic surgery is a minimally invasive procedure using small instruments and a camera that allows orthopedic surgeons to remove scar tissue and release the joint.
These surgical options aim to restore shoulder function and alleviate discomfort. Postoperative rehabilitation is essential to maintain the range of motion gained during the procedure and prevent recurrence.
Recovery Process and Outlook
The recovery process for frozen shoulder can be lengthy, but with appropriate treatment, the outlook is generally very positive. During the thawing stage, shoulder mobility gradually improves over a period ranging from 5 to 24 months, though most individuals see significant recovery within a year. With timely diagnosis and consistent treatment, most patients regain near-normal shoulder function and can return to their usual activities.
Preventing Frozen Shoulder
Preventing frozen shoulder begins with staying proactive about shoulder mobility. Incorporating regular stretching and mobility exercises into your daily routine helps maintain flexibility and joint health. Maintaining good posture during everyday activities is also essential to minimize unnecessary strain on the shoulder joint.
Following any shoulder injury or surgery, early initiation of physical therapy is key to reducing the risk of stiffness and loss of motion. Importantly, paying attention to early signs of discomfort and addressing them promptly can help minor issues from developing into more serious shoulder conditions down the road.
Summary
Frozen shoulder, or adhesive capsulitis, is a complex condition that requires timely intervention and proper management. Understanding the causes, risk factors, symptoms, and treatment options is key to effective recovery. By adopting preventive measures, individuals can support their shoulder health and reduce the risk of developing this condition. Take control of your shoulder health today and embrace a pain-free, mobile future.
Frequently Asked Questions
What is frozen shoulder, and how is it different from a rotator cuff tear?
Frozen shoulder, or adhesive capsulitis, leads to significant stiffness and reduced mobility in the shoulder joint due to inflammation and thickening of the shoulder capsule. A rotator cuff tear, while painful, usually allows some movement and affects different structures within the shoulder.
What are the primary causes of frozen shoulder?
Extended periods of shoulder immobilization, such as following a fracture or surgery, can trigger this condition. Additional risk factors include age (often between 40 and 60), gender (more common in women), and certain medical conditions.
What are the key symptoms of frozen shoulder?
The key symptoms of frozen shoulder are shoulder pain, stiffness, and a notable loss of both active and passive range of motion. This condition typically progresses through three stages: freezing, frozen, and thawing.
How is frozen shoulder diagnosed?
Frozen shoulder is diagnosed through a comprehensive clinical evaluation, which includes a detailed medical history, physical examination, and possibly imaging tests such as X-rays and MRIs to exclude other conditions.
What are the treatment options for frozen shoulder?
The treatment options for frozen shoulder primarily include nonsurgical methods like physical therapy, medications, and injections, while surgical interventions such as shoulder manipulation or arthroscopic surgery are considered if these approaches do not provide relief.