Shoulder joint injections are a common treatment for relieving pain and inflammation in conditions like osteoarthritis, frozen shoulder, and rotator cuff injuries. This post will cover what Shoulder Joint Injection is, who should consider them, and the process involved.
Key Takeaways
- Shoulder joint injections are effective for managing pain from conditions like osteoarthritis and frozen shoulder when conservative treatments fail.
- Proper anatomical knowledge and injection techniques, including anterior, posterior, and ultrasound-guided approaches, are crucial for successful outcomes.
- Post-injection care and monitoring for complications are essential, with corticosteroid injections providing short-term relief but often requiring complementary treatments like physiotherapy for long-term benefits.
Understanding Shoulder Joint Injections
Shoulder joint injections can be a key tool in the management of shoulder pain, particularly for conditions like osteoarthritis, frozen shoulder, and rotator cuff tears. The primary goal of these injections is to reduce pain and inflammation, thereby improving shoulder function and quality of life. Common causes of shoulder pain include rotator cuff pathology, acromioclavicular joint disorders, and glenohumeral joint disorders, often linked to aging or trauma.
These injections should be performed by an experienced orthopedic surgeon. Nonoperative treatments for shoulder pain, such as physical therapy, NSAIDs, and steroid injections, are typically considered first, with injections being a next step when these conservative measures fail.
Anatomy of the Shoulder Joint
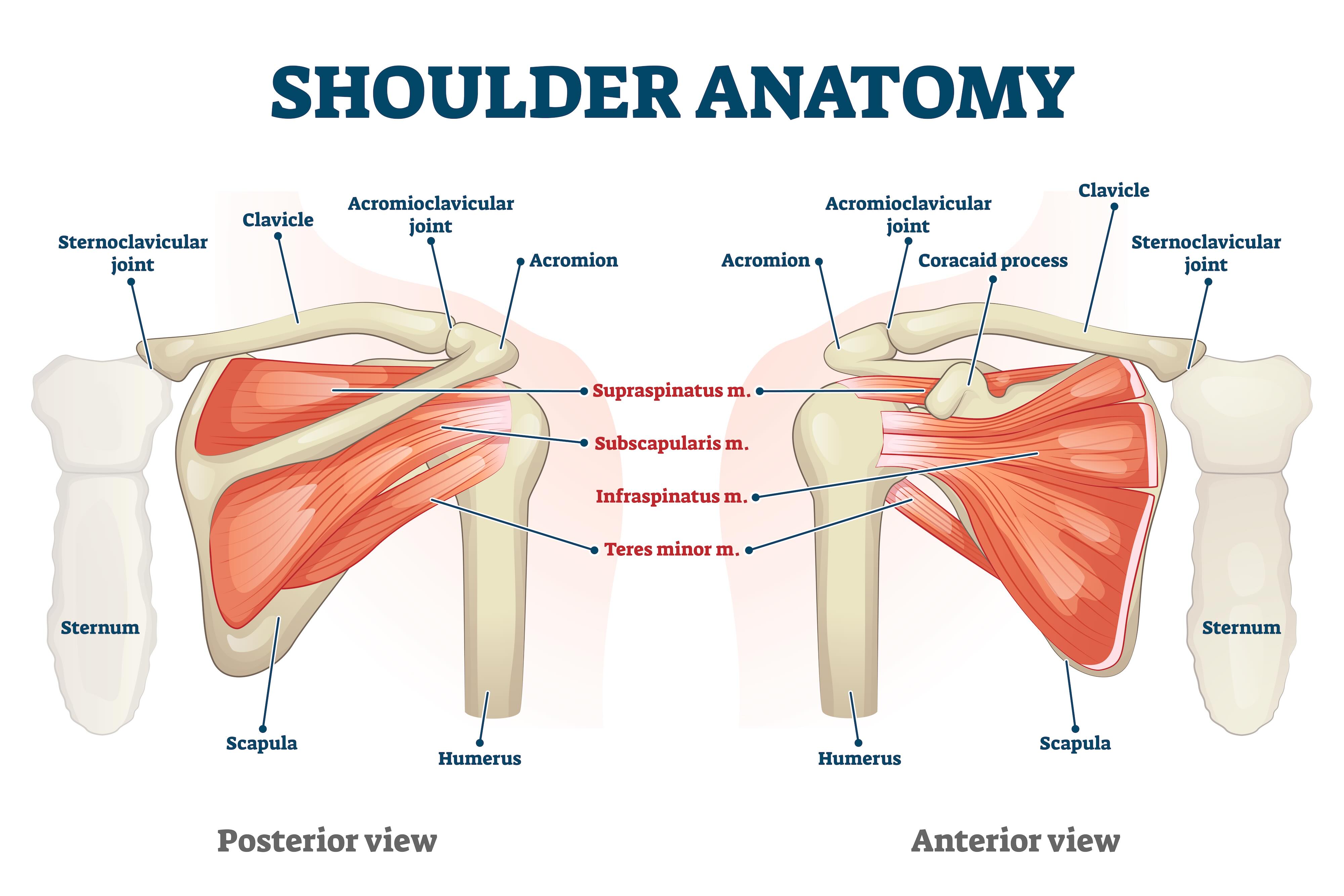
The shoulder joint is a marvel of human anatomy, classified as a ball-and-socket joint, which affords it an extensive range of motion. However, this high mobility comes with a cost: the shoulder’s inherent instability. The glenohumeral joint, a central player in shoulder movement, relies heavily on the surrounding muscles and ligaments for stability and function. The dynamic stabilization of this joint is primarily achieved through the rotator cuff muscles, which are crucial for maintaining shoulder integrity.
The rotator cuff is composed of four muscles: the supraspinatus, infraspinatus, teres minor, and subscapularis. These muscles work in concert to stabilize the glenohumeral joint and facilitate various shoulder movements, such as abduction and rotation.
Apart from the rotator cuff, other critical structures include:
- The joint capsule, a fibrous envelope that surrounds the glenohumeral joint and is pivotal in maintaining joint stability.
- The biceps tendon, particularly the long head, which plays a role in shoulder stability and movement.
- The acromioclavicular joint, located at the top of the shoulder, which connects the acromion and the clavicle and is often implicated in shoulder disorders.
Indications for Shoulder Joint Injections
Shoulder joint injections are indicated for a range of conditions, each presenting unique challenges and requiring targeted treatment.
Common reasons for these injections include:
- Osteoarthritis of the shoulder, characterized by chronic pain, limited motion, and weakness
- Adhesive capsulitis (frozen shoulder)
- Rheumatoid arthritis
- Subdeltoid bursitis
Intra-articular corticosteroid injections are particularly effective for managing adhesive capsulitis and osteoarthritis. These injections help reduce inflammation and pain, providing relief and improving range of motion. Additionally, injections can be used to treat inflammation of the long head of the biceps tendon, rotator cuff tendinosis, and subacromial impingement syndrome.
Pre-Procedure Preparation
Proper preparation significantly contributes to the success of shoulder joint injections. Before undergoing the procedure, patients should first exhaust conservative treatments like NSAIDs and physical therapy. If these measures fail, therapeutic injections become a viable option. Patients need to discuss their medical history, including any allergies, previous reactions to injections, and current medications that could affect bleeding or interact with the injection.
It’s also important to inform the healthcare provider about any active infections, use of antibiotics, or blood thinners, as these can impact the procedure’s safety and efficacy.
On the day of the procedure, patients should eat a light meal and wear loose-fitting clothes or a gown if required. Continuing prescribed medications and bringing a driver to the appointment are also recommended to ensure a smooth and safe process.
Medications Used in Shoulder Joint Injections
Shoulder joint injections utilize various medications to achieve pain relief and reduce inflammation. Commonly used medications include:
- Corticosteroids, such as triamcinolone, which are frequently included in these injections for their long-term anti-inflammatory effects.
- Hyaluronic acid, which helps lubricate the joint and may provide pain relief.
- Platelet-rich plasma (PRP), which is derived from the patient’s own blood and may promote healing.
Corticosteroids help reduce swelling and pain, making them effective for conditions like osteoarthritis and adhesive capsulitis.
Hyaluronic acid (HA) is another option, known for its anti-inflammatory and analgesic properties, though its use in shoulder injections is off-label and not FDA-approved.
PRP therapy, which utilizes the body’s platelets to enhance healing, has shown moderate effectiveness for certain shoulder conditions, reducing inflammation and promoting tissue repair.
Post-Procedure Care
After a shoulder joint injection, proper post-procedure care is essential for optimal recovery and to monitor for any complications. Patients should rest for the first 24 hours and gradually increase activity as tolerated. They can shower the day after the procedure but should avoid soaking in baths or pools for 2-3 days.
To manage any post-injection pain or swelling, patients can apply ice packs during the first 24 hours, followed by warm moist heat. A flare-up of pain and swelling may occur for up to two days following a corticosteroid injection, which is normal.
Scheduling a follow-up appointment within 48 hours helps monitor recovery. Short-term side effects, such as facial flushing and temporary increases in blood sugar levels, may occur but typically resolve on their own.
While shoulder joint injections are generally safe, potential complications and side effects can occur. Patients may experience increased pain for a few days post-injection as the steroid effects take time to manifest. Other mild adverse reactions include facial flushing and menstrual irregularities, particularly in women.
The Role of PRP Injections in Shoulder Treatment
PRP injections have emerged as a promising treatment for various shoulder conditions, including:
- partial-thickness rotator cuff tears
- calcific tendonitis
- adhesive capsulitis
- early glenohumeral arthritis
These injections work by utilizing the body’s platelets to enhance healing, reduce inflammation, and alleviate pain. PRP therapy can provide short-term pain relief and improve range of motion, particularly in cases of adhesive capsulitis.
Typically, a series of two PRP injections are administered, spaced about a month apart. Patients should avoid aggressive activity for the first few days and refrain from taking anti-inflammatories and steroids post-injection.
PRP therapy offers a natural alternative to corticosteroids and can be particularly beneficial for patients looking for non-surgical treatment options.
Summary
In summary, shoulder joint injections are a valuable tool in managing shoulder pain and improving function. Understanding the anatomy of the shoulder, the indications for injections, and the various techniques and medications used can help patients and healthcare providers make informed decisions. By following proper pre-procedure preparations and post-procedure care, and being aware of potential complications, patients can achieve optimal outcomes. Whether choosing corticosteroid injections, physiotherapy, or PRP therapy, the goal remains the same: to reduce pain and enhance quality of life.
Frequently Asked Questions
What conditions of the shoulder have responded favorably to PRP injections?
PRP injections have shown favorable responses in conditions such as partial-thickness rotator cuff tears, calcific tendonitis, adhesive capsulitis, and early glenohumeral arthritis.
What should be avoided after a PRP injection?
After a PRP injection, it is crucial to avoid aggressive activity and refrain from taking anti-inflammatories or steroids for several days to ensure optimal healing.
Does PRP help with frozen shoulder?
Yes, PRP can be beneficial for treating frozen shoulder by promoting healing and reducing pain. Many patients experience improved range of motion following treatment.
How long does adhesive capsulitis typically take to resolve on its own?
Adhesive capsulitis typically takes around one to three years to resolve on its own. However, the duration may vary depending on individual circumstances.
How many PRP injections are typically used to treat shoulder conditions, and how are they spaced?
Typically, two PRP injections are used to treat shoulder conditions, with intervals of approximately one month between each injection.





