Proximal humerus fractures are breaks in the upper arm bone, near the shoulder, commonly caused by falls or direct trauma. Depending on the fracture’s complexity, treatment can range from simple immobilization to surgical repair. In this post, you’ll learn about the types, causes, symptoms, diagnostics, treatment options, and recovery strategies for managing proximal humerus fractures.
Key Takeaways
- Proximal humerus fractures are common injuries classified into various types, which guide treatment and predict recovery outcomes.
- Treatment options vary based on fracture severity and patient health, with non-surgical methods often preferred for less severe cases, while surgical options are for more complex injuries.
- Effective rehabilitation is crucial for recovery, emphasizing early physical therapy, tailored exercise protocols, and adherence to rehabilitation plans to optimize outcomes.
Understanding Proximal Humerus Fractures
Proximal humerus fractures, occurring at the upper part of the humerus bone near the shoulder, are a common injury that can result from various types of trauma. These fractures can be broadly classified using several systems, including the Neer and AO/OTA classifications, which categorize fractures based on the number and type of bone fragments involved. These classifications help determine the appropriate treatment and predict the prognosis for recovery.
The Neer classification, for instance, categorizes proximal humerus fractures into One-Part, Two-Part, Three-Part, Four-Part, Valgus-Impacted Four-Part, Fracture Dislocations, and Articular Surface Injuries. The AO/OTA classification further breaks down these fractures into three main types: Type A (Extraarticular and unifocal), Type B (Extraarticular and bifocal), and Type C (Articular). These classifications allow healthcare providers to tailor treatment strategies to each patient’s specific needs.
Anatomy of the Proximal Humerus
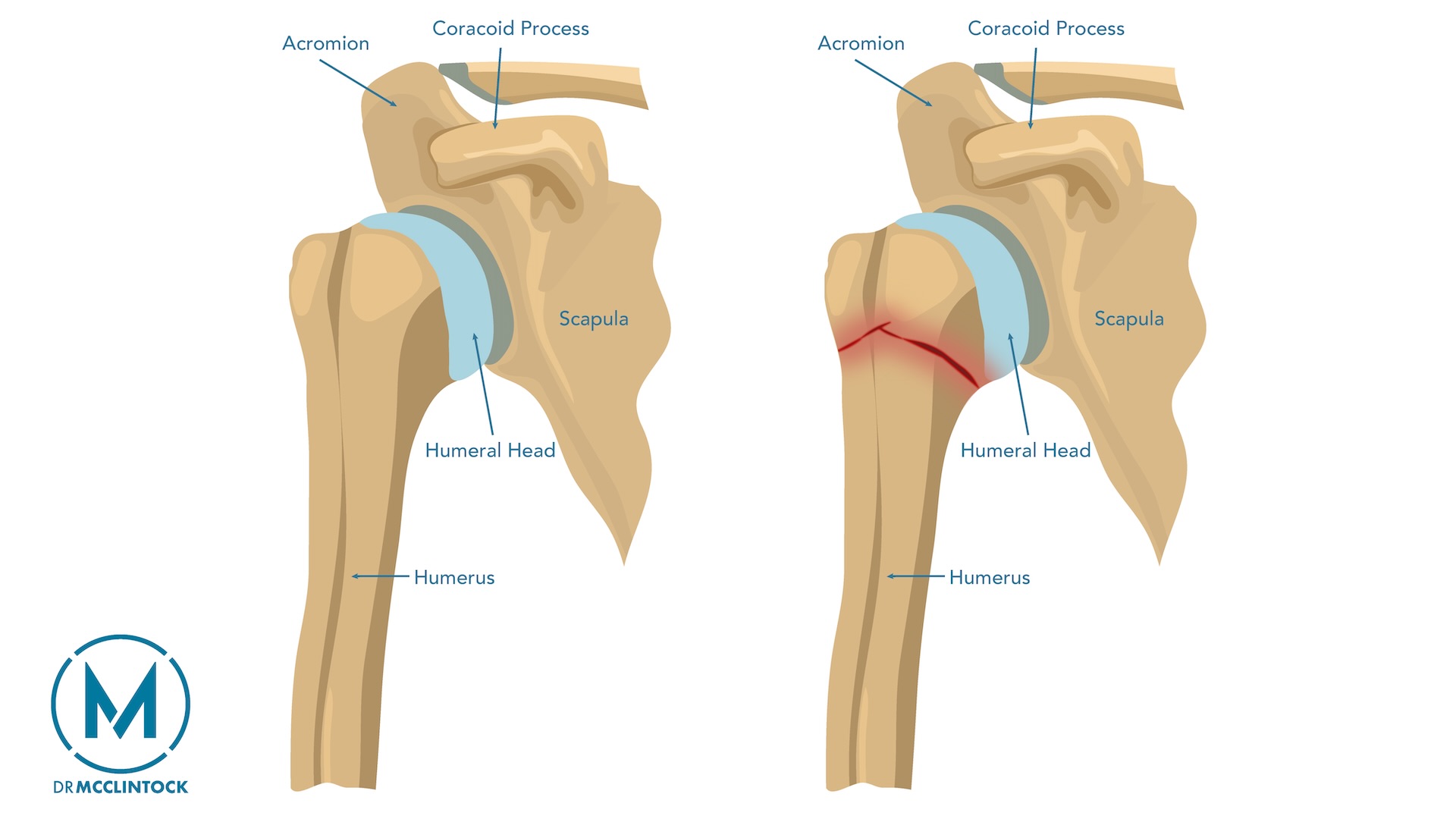
Understanding the anatomy of the proximal humerus is key to grasping the complexities of these fractures. This part of the upper arm bone includes several critical anatomical features, such as the surgical neck and greater tuberosity. The greater tuberosity, in particular, serves as an attachment point for the rotator cuff muscles, which are crucial for shoulder stability and movement.
The proximal humerus facilitates arm movement and rotation, making it crucial for upper limb function. The humeral head articulates with the glenoid fossa of the shoulder blade, forming the shoulder joint, while the anatomical neck separates the humeral head from the shaft of the humerus. This intricate structure allows for a wide range of motion, which is essential for performing daily activities.
Common Causes and Risk Factors
Falls or direct trauma typically cause proximal humerus fractures, resulting in specific patterns of pain and dysfunction. In younger patients, these fractures often occur due to high-energy trauma, such as motor vehicle accidents. However, among older adults, low-energy falls are the most common cause, reflecting the higher prevalence of these fractures in the elderly population.
The average age of patients with proximal humerus fractures is around 70 years, highlighting the increased risk among older individuals.
Several risk factors contribute to this vulnerability, including:
- bone fragility
- low physical activity
- impaired balance
- lower limb pain or injury
These factors not only increase the likelihood of sustaining a fracture but also complicate the recovery process.
Proximal humerus fractures exhibit a bimodal distribution, affecting both younger and older populations through different injury mechanisms. While high-energy trauma is more common in younger patients, older adults are more susceptible due to lower bone density and a higher propensity for falls. This dual pattern underscores the need for tailored prevention and treatment strategies for different age groups.
Clinical Presentation and Diagnosis
Accurate recognition and diagnosis of proximal humerus fractures are crucial steps in managing these injuries. These fractures exhibit a bimodal distribution, occurring due to both high-energy trauma in younger patients and low-energy falls in older adults. They account for about 5% to 6% of all fractures, with a significant prevalence among the elderly.
Associated injuries, such as nerve injuries, particularly axillary nerve injuries, and arterial compromise, can complicate the clinical picture. Recovery outcomes depend heavily on factors like age, fracture type, and adherence to rehabilitation protocols. Accurate diagnosis and timely intervention are essential to ensure optimal recovery and minimize complications.
Symptoms and Physical Examination
Patients with proximal humerus fractures often experience intense shoulder pain, especially during movement, accompanied by visible swelling and bruising. During a physical examination, a shoulder surgeon will look for signs such as open fractures, ecchymosis, crepitus, pain, and loss of deltoid contour. These symptoms provide important clues for identifying the severity and type of fracture.
Assessing the neurological and vascular status of the affected arm is also important. This involves checking for any nerve damage or compromised blood flow, which can significantly impact treatment decisions and outcomes. During the evaluation, the entire limb should be examined to rule out additional fractures beyond the proximal humerus and to assess for humeral head ischemia.
Imaging Techniques
Imaging techniques play a pivotal role in the diagnosis and management of proximal humerus fractures. Plain radiographic imaging, or X-rays, is the primary tool used for this purpose. X-rays provide a clear picture of the bone structure, helping to identify the type and extent of the fracture accurately.
CT scans are used to evaluate the position of the humeral head and plan surgical interventions when more detailed information is needed. These imaging techniques are invaluable in ensuring that the correct diagnosis is made, allowing for effective treatment planning and execution.
Treatment Options for Proximal Humerus Fractures
The type of fracture, extent of bone damage, and the patient’s overall health influence the treatment options for proximal humerus fractures, including displaced proximal humeral fractures. These options can be broadly categorized into non-surgical and surgical management. Whether the fracture is displaced or non-displaced influences the choice of treatment.
Non-surgical management is often preferred for less severe fractures, especially in elderly patients where surgery may not significantly improve functional outcomes. However, when fractures are more complex or involve significant displacement, surgical intervention becomes necessary. Each approach has its own set of benefits and risks, which must be carefully considered to optimize patient outcomes.
Non-Surgical Management
Initial steps in non-surgical management of proximal humerus fractures typically involve immobilization and pain control. Recent evidence suggests that conservative treatment can be just as effective as surgery in improving functional outcomes for elderly patients. A sling is commonly used to hold the shoulder and arm in place, ensuring the glenohumeral joint remains in internal rotation and 0° of adduction during immobilization.
Sling immobilization works well for minimally displaced surgical neck fractures and anatomic neck fractures. Gentle progressive rehabilitation should follow this immobilization. This nonoperative approach has a high success rate, with approximately 80% to 85% of patients achieving satisfactory outcomes.
The duration of splinting or casting varies, typically lasting three to five weeks for mild non-displaced fractures and six to eight weeks for more severe cases.
Surgical Interventions
Surgical interventions are explored when non-surgical management is insufficient, particularly for more severe or displaced fractures. Open reduction and internal fixation (ORIF) is a common surgical technique used to realign and secure the bones for proper healing. This procedure is often recommended for displaced fractures that do not meet criteria for nonoperative management.
In cases where fractures are more complex, particularly in elderly patients with osteoporotic bone or in multi-part fractures (such as 4-part fractures), shoulder replacement (arthroplasty) may be necessary. Shoulder arthroplasty, which can include hemiarthroplasty, total shoulder arthroplasty, or reverse shoulder arthroplasty, is considered when there is a high risk of poor healing or complications, such as avascular necrosis. This procedure is more common in elderly patients, with studies suggesting that 13-30% of severe proximal humerus fractures in this population may require shoulder replacement.
The specific characteristics of the fracture and the patient’s overall health determine the choice of surgical method, with the goal of achieving the best functional outcomes.
Rehabilitation and Recovery
Rehabilitation is important for recovery from proximal humerus fractures. Both surgical and non-surgical treatments require a comprehensive rehabilitation program to restore function and mobility. Long-term recovery often results in satisfactory outcomes and significantly improves the patient’s quality of life.
A tailored rehabilitation plan prevents complications like stiffness and muscle atrophy, ensuring a smoother recovery. Physical therapy is crucial in this phase, with protocols designed to address each patient’s unique needs.
Physical Therapy Protocols
Early physical therapy, ideally within 14 days post-injury, maximizes recovery outcomes. Initial exercises maintain shoulder movement to prevent stiffness and promote healing. Simple movements like finger and wrist exercises are crucial during the early stages while wearing a sling.
Pendulum exercises, involving gentle arm swinging, help regain shoulder mobility. As recovery progresses, active assisted shoulder flexion exercises are introduced around three weeks post-injury to enhance the range of motion further.
Expected Recovery Timeline
Recovery from a proximal humerus fracture typically takes 6 to 12 weeks, depending on injury severity. The first recovery phase after surgical intervention, such as open reduction and internal fixation (ORIF), lasts about 1 to 4 weeks. During this period, the focus is on initial healing and preventing complications.
In the next phase, spanning 4 to 8 weeks, patients gradually increase their range of motion exercises. Around six weeks post-fracture, many patients start to regain normal light activities as healing progresses.
Long-term outcomes are generally positive, with many patients reporting good functional recovery.
Complications and Prognosis
Although many patients recover well from proximal humerus fractures, complications can impact recovery and long-term outcomes. Common concerns include nerve injuries, particularly of the radial nerve, which can occur with humeral shaft fractures but are often reversible. Persistent disability and loss of function are also potential issues.
Age, overall health, and adherence to rehabilitation protocols affect long-term outcomes. Younger patients tend to recover more quickly, while elderly patients may experience more prolonged recovery times and complications.
Potential Complications
Avascular necrosis, nerve damage, and non-union are potential complications of proximal humerus fractures. These issues can significantly affect recovery and overall functional outcomes. Surgical management carries risks like infection and anesthesia-related complications.
Neurovascular injuries, including damage to the axillary nerve and blood vessels, are serious concerns that require careful monitoring and management. These complications underscore the need for a comprehensive treatment plan addressing all aspects of the injury.
Long-Term Outcomes
Long-term outcomes for proximal humerus fractures vary based on factors such as the patient’s age, overall health, and adherence to rehabilitation protocols. Younger patients often have a more straightforward recovery, with symptoms improving within a few weeks post-treatment. This rapid improvement is typically due to better bone quality and a more robust healing response.
In contrast, elderly patients may have a longer and more challenging recovery process. Despite these challenges, many patients can begin moving again within a few weeks of treatment, gradually regaining their normal activities over time. Adhering to rehabilitation protocols is critical for achieving the best functional outcomes and minimizing long-term disability risk.
Prevention Strategies
Preventing proximal humerus fractures is essential, especially for high-risk groups like the elderly. Regular exercise routines can significantly strengthen muscles and enhance balance, reducing the risk of falls and fractures. Exercise to improve strength and balance is key to lowering fall risk, a common cause of proximal humerus fractures.
Encouraging high-risk individuals to adopt these exercise regimes can play a crucial role in preventing serious injuries, including proximal humerus fractures. Additionally, educating patients about proper fall prevention techniques and maintaining good bone health are crucial steps in reducing the incidence of these fractures.
Fall Prevention Tips
Balance and strength training exercises can help elderly patients maintain stability and reduce fall risk. Regular vision and hearing check-ups are also important, as minor changes in these senses can increase the likelihood of falls in older adults.
Assistive devices like canes or walkers can provide added stability and prevent falls among elderly individuals. Fall prevention is about maintaining independence and quality of life for elderly patients, not just avoiding injuries.
Bone Health Maintenance
Maintaining good bone health is crucial for preventing fractures, especially in vulnerable populations like the elderly. Regular weight-bearing exercises like walking or light resistance training promote bone density and prevent osteoporosis-related fractures. At least 150 minutes of weekly physical activity contributes to overall bone health and can reduce fracture risk.
A balanced diet rich in calcium and vitamin D is vital for maintaining strong bones. Encouraging patients to adopt these healthy habits can significantly reduce the risk of sustaining a proximal humerus fracture and improve overall quality of life.
Summary
In conclusion, proximal humerus fractures are complex injuries that require a comprehensive approach to treatment and recovery. Understanding the anatomy, causes, and risk factors of these fractures is essential for accurate diagnosis and effective management. Both non-surgical and surgical treatment options have their place, depending on the severity of the fracture and the patient’s overall health.
Rehabilitation and recovery are critical components of the healing process, with physical therapy playing a vital role in restoring function and mobility. Preventing these fractures through regular exercise, fall prevention strategies, and maintaining good bone health is equally important. By applying the knowledge gained from this post, patients, caregivers, and healthcare professionals can work together to achieve the best possible outcomes.
Frequently Asked Questions
What are the common causes of proximal humerus fractures?
Proximal humerus fractures commonly occur due to falls or direct trauma, with younger individuals usually facing high-energy incidents like motor vehicle accidents, while older adults are more likely to sustain fractures from low-energy falls.
How are proximal humerus fractures diagnosed?
Proximal humerus fractures are diagnosed through a combination of physical examination and imaging techniques, primarily X-rays, and sometimes CT scans, to determine the type and extent of the injury. This thorough approach ensures accurate assessment for optimal treatment.
What are the treatment options for proximal humerus fractures?
The treatment options for proximal humerus fractures include both non-surgical methods, such as immobilization and rehabilitation, and surgical interventions like open reduction and internal fixation (ORIF) or shoulder replacement. Choosing the appropriate approach depends on the fracture’s severity and the patient’s overall health.
What role does physical therapy play in recovery?
Physical therapy is essential for recovery as it prevents stiffness and promotes healing through targeted exercises that maintain flexibility and gradually enhance the range of motion. Engaging in physical therapy can significantly improve your overall recovery process.
How can proximal humerus fractures be prevented?
To prevent proximal humerus fractures, it is essential to engage in regular exercise to strengthen muscles and enhance balance while also focusing on maintaining good bone health through a balanced diet and weight-bearing activities. Implementing fall prevention strategies is crucial to minimizing the risk of injury.