Osteonecrosis of the shoulder occurs when the blood supply to the humeral head is disrupted, leading to bone death. This can cause significant shoulder pain and limited mobility.
In this post, we will explore the causes, symptoms, and treatment options for osteonecrosis shoulder to help you understand and manage this condition.
Key Takeaways
- Osteonecrosis of the shoulder typically results from disrupted blood supply, often due to trauma, corticosteroid use, sickle cell disease, or heavy alcohol consumption.
- Timely and effective diagnosis is crucial, involving clinical evaluations and imaging techniques like MRI to identify the condition before significant progression occurs.
- Treatment options vary from conservative measures and core decompression for early-stage disease to surgical interventions like shoulder arthroplasty for advanced cases, emphasizing the importance of early detection and intervention.
Vascular Anatomy of the Shoulder
The vascular anatomy of the shoulder is key to understanding how osteonecrosis develops. The shoulder’s blood supply primarily comes from the anterior and posterior humeral circumflex arteries, which stem from the axillary artery. These arteries supply blood to the shoulder joint and surrounding tissues, maintaining the health and function of the shoulder.
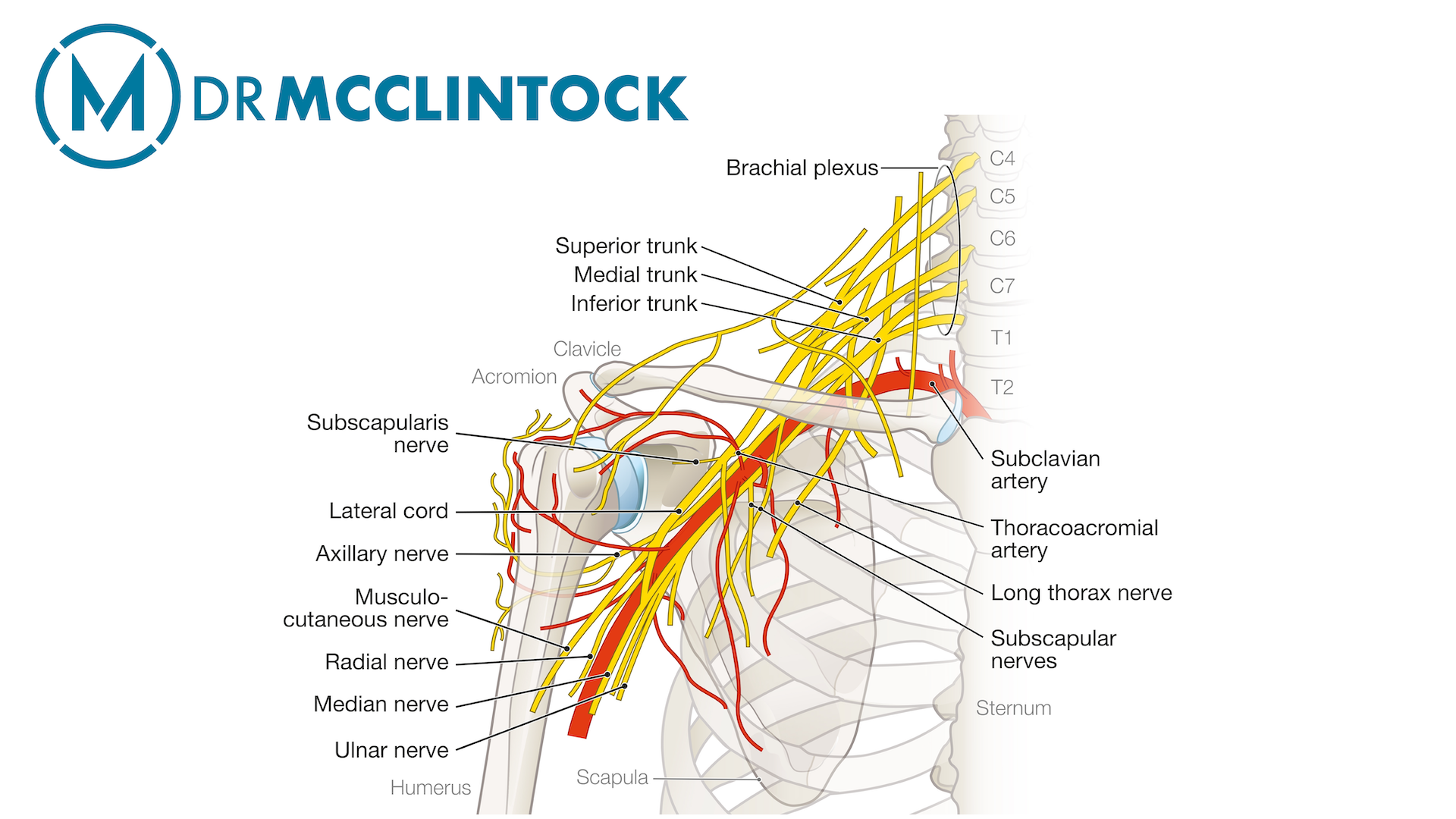
The anterior humeral circumflex artery specifically supplies blood to the shoulder joint. Any disruption in its flow can lead to severe consequences, including osteonecrosis of the humeral head. The posterior humeral circumflex artery primarily supplies the humeral head and surrounding tissues, ensuring their vitality and health.
Moreover, the shoulder’s blood vessels, including the arcuate artery and the ascending branch, work together to ensure a robust vascular supply to the proximal humerus and humeral head. Disruptions in this network can lead to humeral head avascular necrosis, highlighting the need to understand this anatomy for diagnosing and treating shoulder osteonecrosis.
Common Causes of Osteonecrosis in the Shoulder
Osteonecrosis of the shoulder can be triggered by various factors, each affecting the blood supply to the humeral head differently. One of the most common causes is trauma, which can disrupt blood flow and lead to bone death.
Other significant causes include long-term corticosteroid use, which can result in fat cell hypertrophy and decreased blood flow, and sickle cell disease, known for causing vascular blockages and reducing blood flow.
Additionally, heavy alcohol consumption is a recognized cause of osteonecrosis, with a clear dose-response relationship indicating increased risk with higher alcohol intake.
Knowing these causes aids in both preventing and managing the progression of shoulder osteonecrosis.
Trauma-Induced Osteonecrosis
Trauma-induced osteonecrosis is a significant concern, especially following severe injuries that can disrupt blood flow to the shoulder. When the blood supply to the humeral head is compromised, it can lead to avascular necrosis and subsequent bone death. This disruption often results in symptomatic humeral head osteonecrosis, characterized by shoulder pain and limited mobility.
In many cases, trauma-induced osteonecrosis can progress rapidly, necessitating early intervention and management to prevent extensive damage. Being aware and seeking prompt treatment after shoulder injuries can help reduce the risk of this debilitating condition.
Corticosteroid Use and Osteonecrosis
Corticosteroid use is another well-documented cause of osteonecrosis of the humeral head. Prolonged corticosteroid therapy can lead to fat accumulation in the bone marrow, resulting in decreased blood flow and eventually osteonecrosis. Steroid-induced osteonecrosis underscores the need to monitor corticosteroid use closely.
Patients on long-term corticosteroid therapy should be aware of the risks and collaborate with their healthcare providers to manage dosages and treatment duration. Early detection and intervention can halt the progression of symptomatic humeral head osteonecrosis, preserving shoulder function and quality of life.
Sickle Cell Disease and Bone Death
Sickle cell disease significantly impacts the vascular system, leading to complications like bone death. The abnormal shape of sickle cells causes vascular blockages, reducing blood flow to critical areas like the humeral head. This decreased blood flow can result in osteonecrosis, often progressing silently until advanced stages.
Regular monitoring for signs of osteonecrosis is necessary for patients with sickle cell anemia. Early diagnosis and intervention are crucial in managing disease progression and maintaining shoulder joint health, preventing severe complications and disability.
Alcohol and Blood Flow Disruption
Heavy alcohol consumption is a known risk factor for osteonecrosis due to its impact on blood supply. Alcohol can impair blood flow to the shoulder joint, significantly increasing the risk of osteonecrosis. Studies have shown a clear dose-response relationship, with higher alcohol intake correlating with a higher risk of developing the condition.
Reducing alcohol intake can significantly lower the risk of osteonecrosis for heavy drinkers. Lifestyle modifications, including managing alcohol consumption, play an important role in preventing this debilitating condition and maintaining overall joint health.
Clinical Evaluation and Diagnosis
Clinical evaluation and diagnosis of osteonecrosis are critical steps in managing the condition effectively. Osteonecrosis arises when a portion of the bone loses its blood supply, leading to tissue death and subsequent shoulder pain. Common symptoms include poorly localized shoulder pain and limitations in daily activities, which can significantly impact quality of life.
Identifying high-risk individuals is key to implementing effective preventive strategies for osteonecrosis. Patients with atraumatic osteonecrosis of the humeral head are usually asymptomatic until the later stages, making early diagnosis challenging. However, even advanced stages can present minimal symptoms, necessitating vigilance in at-risk populations.
Radiographic assessments and laboratory tests are crucial for diagnosing osteonecrosis and identifying underlying conditions like sickle cell disease or hyperlipidemia. Educating patients about osteonecrosis symptoms and risk factors can lead to earlier diagnosis and better management, improving long-term outcomes.
Imaging Techniques for Early Diagnosis
Imaging techniques play a crucial role in the early diagnosis of osteonecrosis. Radiographic imaging is often the first step, requiring specific views like anteroposterior and axillary to identify changes. However, when radiographs show no abnormalities, MRI becomes the preferred diagnostic tool due to its high sensitivity and specificity.
MRI evaluations can reveal critical indicators of osteonecrosis, such as the double line sign on T2-weighted images and band-like abnormal signals, which are crucial for early detection. Low signal serpiginous lines on T1-weighted images further suggest the presence of osteonecrosis, providing valuable insights for diagnosis.
For patients at risk of advanced osteonecrosis, MRI can offer valuable insights for early diagnosis and management, potentially preventing disease progression and preserving shoulder function.
Staging and Prognosis of Shoulder Osteonecrosis
The staging and outlook for shoulder osteonecrosis are important for figuring out the best treatment. Doctors often use a system called the modified Ficat and Arlet classification to measure how severe the disease is. Another system, called the Cruess classification, breaks down the progression of the condition into five stages, based on X-rays and MRI scans.
Stage 1: X-rays look normal, but an MRI shows abnormal signals in the bone.
Stage 2: X-rays may show some hardening of the bone, but the shape of the humeral head (the top of the arm bone) is still fine.
Stage 3: A “crescent sign” appears on X-rays, showing early damage to the bone under the joint surface.
Stage 4: There’s noticeable damage to the joint surface, and loose pieces of bone may be floating inside the joint.
Stage 5: The joint shows advanced damage and no longer fits together properly.
MRIs can help predict how likely the bone in the shoulder is to collapse, which affects the prognosis and treatment decisions. For people in the early stages (Stages 1 and 2), a procedure called core decompression can lead to good results in about 90% of cases, giving hope for effective treatment early on.
Conservative Treatment Options
Conservative treatment is often the first line of defense for patients with atraumatic humeral head osteonecrosis. Physical therapy is a key non-surgical approach, helping to improve shoulder function and alleviate pain in early-stage disease. Pain management frequently involves the use of non-steroidal anti-inflammatory drugs (NSAIDs), which can help reduce discomfort and inflammation.
Modifying activities to reduce strain on the shoulder joint is another important aspect of conservative treatment. Timely intervention with non-surgical methods can prevent avascular necrosis progression, preserving shoulder health and function.
Surgical Interventions for Advanced Disease
For advanced osteonecrosis of the shoulder, surgical interventions become necessary. These include core decompression, arthroscopic-assisted techniques, and shoulder arthroplasty. Many adults with symptomatic humeral head osteonecrosis related to sickle cell disease require surgical treatment.
Favorable postoperative outcomes are linked to specific preoperative conditions. These include mild to moderate pain, preserved range of motion (ROM), and minimal delay to surgery, underscoring the necessity of timely surgical intervention.
Core Decompression Techniques
Core decompression is a frequently used surgical technique for early-stage osteonecrosis. It is indicated for Stage 1 and 2 Osteonecrosis and sometimes recommended in Stage 3 if there is minimal subchondral fracture. The primary aim is to reduce intraosseous pressure and restore circulation, which can significantly improve outcomes.
The success rate of core decompression in Stage 1 shoulders is reportedly high, around 94%.
For early-stage avascular osteonecrosis of the humeral head, fluoroscopy-guided core decompression, with or without bone grafting, is a viable option if conservative treatment fails.
Arthroscopic-Assisted Treatments
Arthroscopic-assisted treatments provide a minimally invasive option for managing osteonecrosis. Arthroscopic management aims to preserve the joint, limiting damage and recovery time.
In some cases, arthroscopic debridement has improved range of motion and reduced symptoms, especially in Stage 3 Osteonecrosis. Techniques such as autologous bone graft and bone morphogenetic protein application can further enhance the effectiveness of these treatments.
Shoulder Replacement
Shoulder replacement is typically reserved for patients with advanced osteonecrosis of the humeral head. Total shoulder arthroplasty is indicated for those experiencing severe arthritis and significant joint damage.
Successful shoulder replacements can lead to significant improvements in patient outcomes, including pain reduction and enhanced shoulder function post-surgery. This makes shoulder replacement surgery a valuable option for advanced osteonecrosis patients.
Preventive Measures and Risk Reduction
Preventive measures and risk reduction strategies are crucial in managing osteonecrosis. Assessing the dose and duration of corticosteroid treatment can lower the risk of developing osteonecrosis. High levels of alcohol consumption are also correlated with an increased risk, so reducing intake can significantly decrease the likelihood of osteonecrosis.
Maintaining a healthy weight and regular physical activity support overall joint health, potentially reducing osteonecrosis risks. Lifestyle modifications play a pivotal role in preventing this debilitating condition and ensuring long-term shoulder health.
Summary
In summary, understanding the vascular anatomy of the shoulder and the common causes of osteonecrosis is essential for early diagnosis and effective management. Imaging techniques such as MRI are invaluable in detecting early-stage disease, while conservative treatments can prevent progression in many cases. For advanced disease, surgical interventions offer hope for improved outcomes and pain relief.
Preventive measures, including lifestyle modifications and careful management of corticosteroid use, are key to reducing the risk of osteonecrosis. By staying informed and proactive, individuals can take control of their shoulder health and minimize the impact of this condition.
Frequently Asked Questions
What is osteonecrosis of the shoulder?
Osteonecrosis of the shoulder is a condition where bone tissue dies due to inadequate blood supply, resulting in pain and reduced mobility. Addressing this issue promptly is crucial for maintaining shoulder function.
What are the common causes of shoulder osteonecrosis?
Shoulder osteonecrosis is commonly caused by trauma, long-term corticosteroid use, sickle cell disease, and heavy alcohol consumption. Identifying these risk factors is crucial for prevention and management.
How is shoulder osteonecrosis diagnosed?
Shoulder osteonecrosis is diagnosed through a combination of clinical evaluation, radiographic imaging, and MR. Early imaging is important for effective diagnosis and management.
What are the treatment options for shoulder osteonecrosis?
The treatment options for shoulder osteonecrosis include conservative methods like physical therapy and NSAIDs, as well as surgical interventions such as core decompression, arthroscopic-assisted treatments, and shoulder arthroplasty. It’s important to consult an orthopedic shoulder surgeon to determine the best approach tailored to individual needs.
How can I prevent osteonecrosis of the shoulder?
To prevent osteonecrosis of the shoulder, focus on reducing alcohol intake, managing corticosteroid use, maintaining a healthy weight, and staying physically active. These lifestyle changes can significantly lower your risk.