Osteoporosis weakens bones, making them fragile, while osteoarthritis affects joints, causing pain and stiffness. In this post, we’ll examine how these conditions differ, including their symptoms and treatment options.
Key Takeaways
- Osteoporosis is characterized by reduced bone density, leading to brittle bones and fractures. Osteoarthritis is a degenerative joint disease that causes cartilage degradation and joint pain.
- Key risk factors for osteoporosis include age, gender, and family history, whereas osteoarthritis risk factors include obesity, prior joint injuries, and repetitive stress on joints.
- Effective management of both conditions, depending on severity, may involve lifestyle changes, proper nutrition, medications, and/or surgery.
Osteoporosis and Osteoarthritis: An Overview
Osteoporosis and osteoarthritis are two prevalent conditions that significantly impact bone health and joint functionality. These conditions are commonly confused with one another, as both affect the skeletal system. However, they are fundamentally different.
Over 200 million people worldwide are affected by osteoporosis, which weakens bones by reducing their density, leading to increased fracture risk. Osteoarthritis, on the other hand, is a degenerative joint disease that primarily affects cartilage, resulting in joint pain, stiffness, and inflammation. While both conditions become more common with age, they require distinct diagnosis and treatment approaches.
What is Osteoporosis?
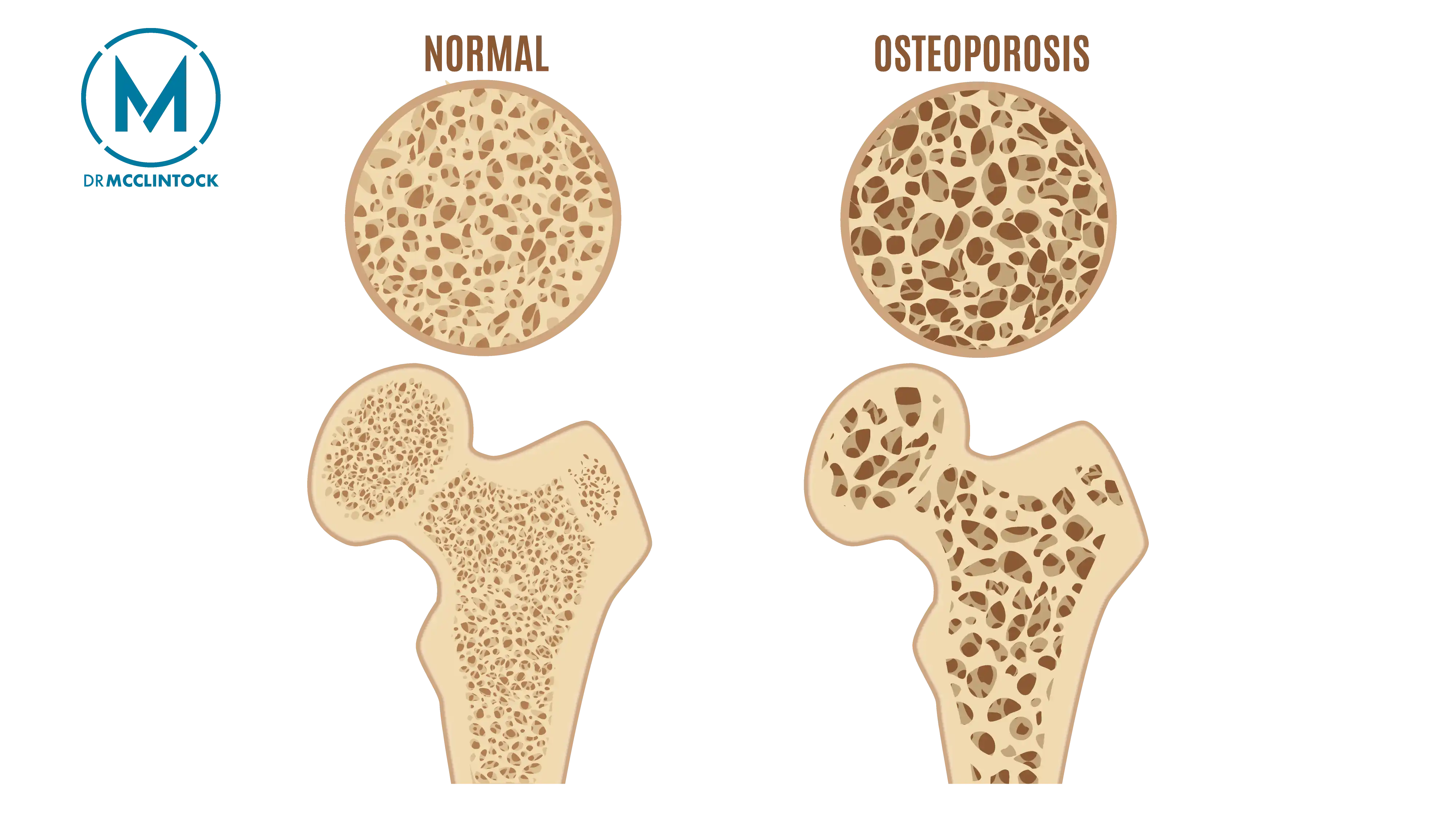
Osteoporosis, meaning “porous bone,” occurs when bone loss exceeds bone formation, reducing density and weakening the skeletal structure. This imbalance makes bones more brittle and prone to fractures, especially in areas like the hips, shoulders, spine, and wrists. Postmenopausal women are at higher risk due to hormonal shifts that accelerate bone density loss.
One of the challenges with osteoporosis is that it often remains undetected until a fracture occurs, earning it the nickname “silent disease.” Common symptoms include back pain and a stooped posture, caused by spinal fractures and compression.
Prioritizing bone health through nutrition and exercise can help prevent osteoporosis and reduce the risk of fractures.
What is Osteoarthritis?
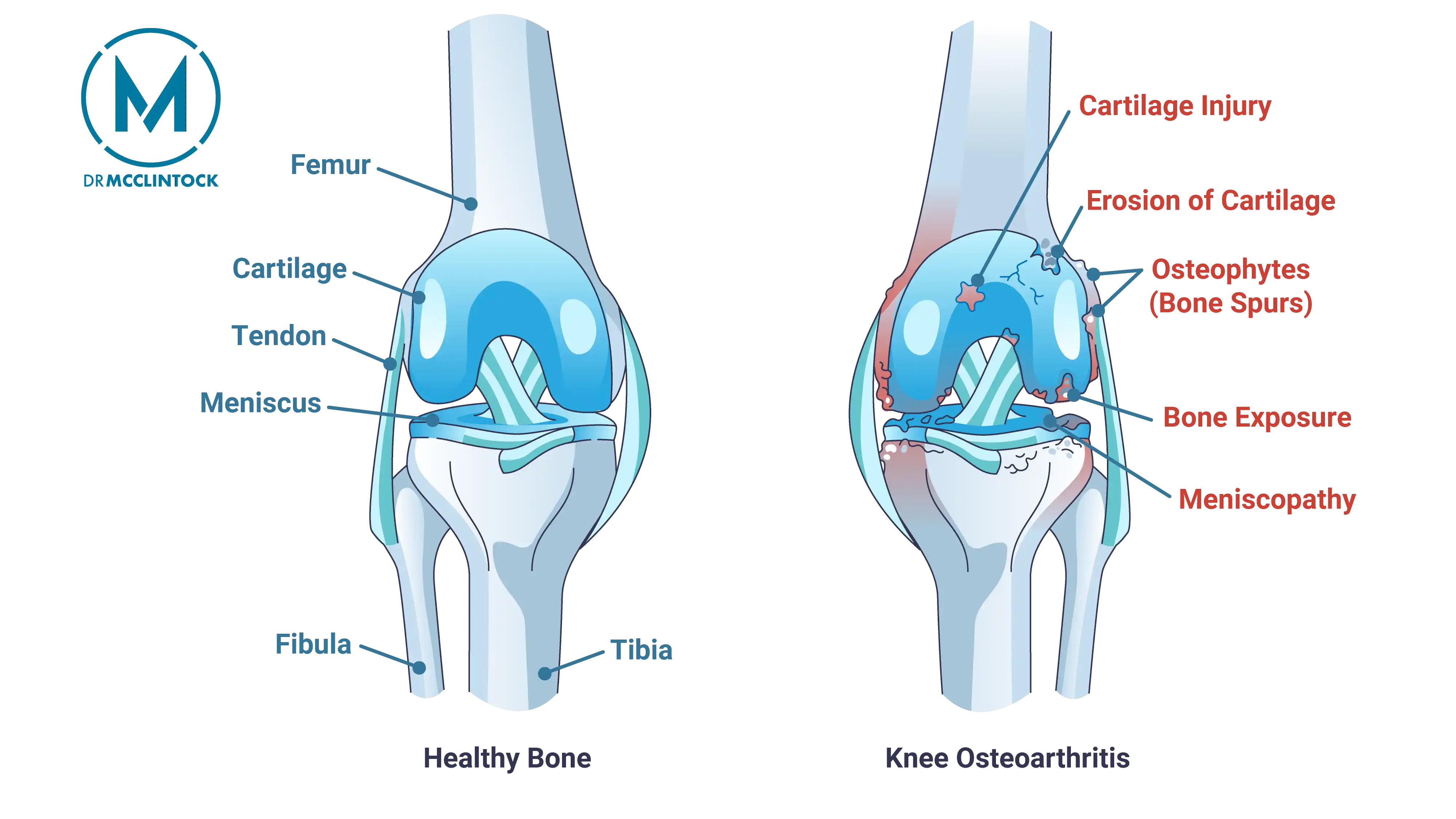
Osteoarthritis is a degenerative joint disease where cartilage breaks down, causing pain, inflammation, and eventual bone-on-bone contact in affected joints. Unlike osteoporosis, which targets bones, osteoarthritis specifically damages joints.
Commonly affected areas include:
- Shoulders
- Hands
- Knees
- Hips
- Lower back
- Spine
- Neck
While most cases are seen in adults over the age of 50, younger individuals with prior joint injuries can also develop this condition.
Management of osteoarthritis involves addressing joint pain and inflammation through a combination of lifestyle changes, medications, and physical therapy.
Key Differences Between Osteoporosis and Osteoarthritis
Osteoporosis and osteoarthritis, while both affecting the musculoskeletal system, differ significantly in their impact and management approaches. The symptoms, risk factors, and treatments are distinct, highlighting the need for targeted approaches to each condition.
Affected Areas
Osteoporosis most frequently leads to fractures in weight-bearing bones such as the spine and hips, due to loss of bone density that results in porous bones. The structural integrity of bones is compromised, making them susceptible to breaks even from minor falls or stresses.
On the other hand, osteoarthritis primarily affects the cartilage within joints, leading to painful bone-on-bone contact. The affected joints often include the shoulder, hands, knees, hips, and spine, impacting overall mobility and quality of life.
Symptoms Comparison
Osteoporosis typically progresses without noticeable symptoms until a fracture happens, earning its reputation as a silent disease. Common symptoms include sudden back pain from spine fractures and a stooped posture.
In contrast, osteoarthritis presents symptoms early, with joint pain, inflammation, and stiffness being the most prevalent. The inflammatory nature of osteoarthritis may lead to visible joint swelling and discomfort that radiates to surrounding areas. For example, a patient may feel pain in the groin and inner thigh when the hips are affected.
Early recognition of these distinct symptom patterns can enable more timely and appropriate management of both conditions.
Risk Factors
The risk factors for osteoporosis and osteoarthritis share some similarities but contain important distinctions.
For osteoporosis, age, gender, and family history significantly increase the risk. Postmenopausal women are especially susceptible. Osteoarthritis risk factors include genetic predisposition, obesity, prior joint injuries, and repetitive stress on the joints.
Both conditions have controllable risk factors that can be addressed through lifestyle modifications. Routine screening and targeted interventions like nutrition, exercise, and weight management can help manage these risks and prevent the progression of osteoporosis and osteoarthritis.
Understanding Risk Factors
Recognizing the risk factors for osteoporosis and osteoarthritis is essential for early intervention and effective management. Both conditions reward proactive measures.
Osteoporosis Risk Factors
Osteoporosis risk factors include both uncontrollable and controllable elements. Uncontrollable factors such as age, gender, and family history play a significant role. The risk of developing osteoporosis increases significantly for individuals over age 50, with half of women over 65 affected by the condition. Hormonal factors like early menopause and lack of estrogen further elevate the risk.
Controllable risk factors include:
- Diet: A diet low in calcium and Vitamin D can negatively impact bone health.
- Physical activity levels: Regular physical activity and maintaining a healthy weight can minimize osteoporosis risk.
- Alcohol consumption and smoking: Both excessive alcohol consumption and smoking are known to decrease bone density and should be avoided.
Osteoarthritis Risk Factors
As people age, the risk of developing osteoarthritis increases significantly. Obesity is another significant risk factor, as excess weight places additional stress on joints, accelerating cartilage degradation. Previous joint injuries and repetitive stress also contribute to the development of osteoarthritis.
Lifestyle changes, such as maintaining a healthy weight and avoiding activities that stress the joints, can help reduce the risk.
Recognizing Symptoms
Early symptom recognition differentiates osteoporosis from osteoarthritis and enables timely care. Regular physical examinations and routine screenings are key to detecting these conditions early and preventing further complications.
Osteoporosis Symptoms
Most people discover they have osteoporosis after experiencing a bone fracture. Fractures most often occur in the hips, spine (vertebrae), and wrists. The shoulder is another common site for osteoporotic fractures due to its wide range of motion and the demands placed on its supporting structures. Other symptoms, like a stooped posture and sudden back pain due to spine fractures, may also manifest.
Osteoarthritis Symptoms
Common symptoms of osteoarthritis include joint pain and stiffness, which often vary in intensity and can be accompanied by swelling. Pain can occur in various areas such as the groin, inner thigh, and neck, particularly if the hips are affected. The joints commonly affected by osteoarthritis include the shoulder, neck, hands, back, hips, knees, and spine.
Unlike osteoporosis’s silent damage, these symptoms often impact daily activities and quality of life.
Treatment Options
Effective management of osteoporosis and osteoarthritis requires a multi-faceted approach tailored to each condition’s pathology. While both benefit from exercise and lifestyle modifications, their medical treatments target different processes: bone preservation for osteoporosis and joint protection for osteoarthritis.
By adopting a comprehensive treatment plan, patients can effectively manage their condition and improve their overall quality of life.
Osteoporosis Treatments
The primary goals of osteoporosis treatment are to preserve bone density and prevent fractures. Medical options include hormone replacement therapy (particularly estrogen for postmenopausal women) and bone-building medications like teriparatide for severe cases.
Lifestyle changes also play a key role in treatment and prevention. Weight-bearing exercises and strength training can enhance bone density and muscle mass. Calcium and vitamin D supplements are often recommended to support bone health.
Osteoarthritis Treatments
Osteoarthritis management focuses on pain relief, inflammation control, and joint preservation. Pain management medications for osteoarthritis treatment include anti-inflammatory medications and analgesics. Over-the-counter topical and oral medications, as well as steroids, can also help manage symptoms.
A home exercise program is often recommended to strengthen muscles around the joints and reduce pain. Weight management helps to alleviate symptoms by reducing stress on affected joints. Initial management strategies include modifying daily activities and engaging in physical therapy to stabilize joints and increase flexibility.
When conservative measures fail, joint replacement surgery may be considered to offer pain relief and restore function. Surgical interventions for shoulder arthritis range from arthroscopic debridement to shoulder replacement, depending on severity.
Maintaining Bone and Joint Health
Prioritizing bone and joint health helps to prevent and manage both osteoporosis and osteoarthritis. A dual-focused approach incorporating proper nutrition and regular physical activity forms the cornerstone of prevention and management for these conditions. By adopting these practices, individuals can prevent the onset of these conditions and improve their overall well-being.
Nutrition for Bone Health
Optimal bone strength requires nutritional building blocks, specifically calcium and vitamin D. Excellent dietary sources of calcium include dairy products and leafy greens. Vitamin D can be found in fatty fish, egg yolks, and certain fortified foods. Postmenopausal women should aim for a daily calcium intake of 1,200 mg and 800 international units (20 mcg) of vitamin D. Calcium and vitamin D supplements are often recommended for osteoporosis.
A balanced diet rich in these nutrients serves as both treatment and prevention for bone density loss.
Exercise for Joint Health
A tailored exercise regimen addresses both conditions simultaneously. Reaching and maintaining a healthy weight is essential for promoting joint and bone health. Low-impact exercises such as walking or cycling are recommended for maintaining joint health in osteoarthritis patients.
An overall fitness routine should include strengthening, cardio, balance, and stretching exercises for optimal results. Patients, especially those with existing joint damage or osteoporosis, should consult a doctor before starting a new routine to avoid injury while maximizing benefits.
When to Consult an Orthopedic Surgeon
Timely medical consultation helps to prevent complications in both conditions. Warning signs prompting immediate evaluation include height loss or postural changes and joint pain limiting function. Emergency medical attention is necessary if an individual suspects a broken bone or experiences severe symptoms like intense pain or inability to move a body part.
Regular screening for osteoporosis is recommended, typically conducted during health exams and lasting about 5-10 minutes. If you have concerns about osteoporosis or osteoarthritis, contact an orthopedic surgeon for guidance.
Summary
Osteoporosis and osteoarthritis, while they both affect the musculoskeletal system, are distinct conditions that require distinct treatment approaches. While osteoporosis affects bone density, leading to increased fracture risk, osteoarthritis impacts joint structures, causing pain and reduced mobility. Recognizing the symptoms and understanding the risk factors for both conditions can lead to early intervention and improved outcomes.
By maintaining a balanced diet rich in calcium and vitamin D, engaging in regular weight-bearing exercises, and seeking timely medical advice, individuals can manage their bone and joint health effectively. Remember, proactive measures and informed decisions are key to preventing and managing osteoporosis and osteoarthritis.
Frequently Asked Questions
What are the main differences between osteoporosis and osteoarthritis?
Osteoporosis primarily reduces bone density, leading to increased fracture risk, whereas osteoarthritis erodes joint cartilage, resulting in pain and inflammation. This fundamental difference dictates their prevention and treatment strategies.
What are common symptoms of osteoporosis?
Osteoporosis is known as a “silent disease,” as it typically presents no symptoms until a fracture occurs. Other signs may include sudden back pain from spinal fractures and a stooped posture.
How can I reduce my risk of developing osteoporosis?
To effectively reduce your risk of developing osteoporosis, focus on a balanced diet high in calcium and vitamin D, incorporate regular weight-bearing exercises into your routine, and limit alcohol intake and smoking. Making these lifestyle adjustments can significantly enhance your bone health.
What are the common treatment options for osteoarthritis?
Common treatment options for osteoarthritis include medications, physical therapy, lifestyle modifications, weight management, and, in severe cases, joint replacement surgery. These approaches can help manage symptoms and improve quality of life.
When should I consult a doctor about osteoporosis or osteoarthritis?
You should consult a doctor if you experience symptoms like joint pain, stiffness, decreased height, sudden back pain, or altered posture, as these may indicate osteoporosis or osteoarthritis. Additionally, consider regular screenings for osteoporosis to stay proactive about your bone health.





