Wondering if carpal tunnel syndrome can come back post-surgery? Some patients experience a recurrence of symptoms long after their initial procedure. In this post, we’ll explore why this happens and the key factors involved.
Key Takeaways
- Incomplete decompression or scar tissue formation from the initial surgery can lead to recurrent carpal tunnel syndrome, affecting roughly 20% of patients.
- Symptoms may reappear anywhere from 1 month to 5 years post-surgery, with risk factors linked to pre-existing medical conditions and anatomical differences.
- Both non-surgical and surgical treatments are available for managing recurrent symptoms, and prevention strategies such as ergonomic adjustments and regular breaks can reduce recurrence risks.
Understanding Carpal Tunnel Syndrome
Carpal tunnel syndrome is caused by the compression of the median nerve within the wrist’s carpal tunnel. This pressure can lead to symptoms like tingling, numbness, and weakness, particularly in the thumb and the first three fingers. The symptoms often start gradually and worsen over time, making daily tasks increasingly difficult.
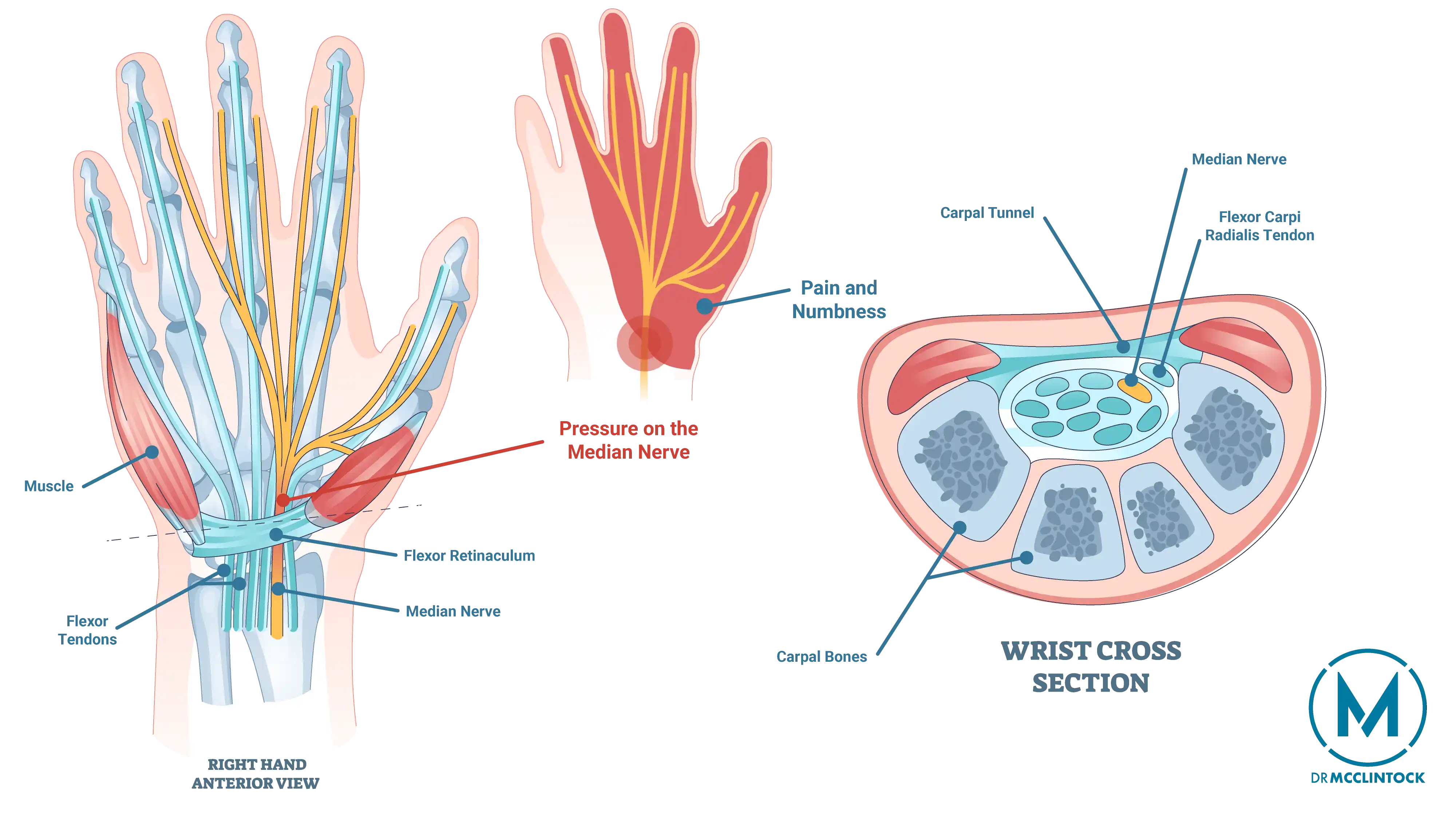
Women are generally at a higher risk of developing carpal tunnel syndrome, potentially due to having smaller carpal tunnel anatomy. While the condition is not usually painful, the tingling and numbness can become quite bothersome, especially if untreated. Over time, hand weakness may develop, leading to difficulties with gripping and holding objects.
While these fundamentals explain how carpal tunnel syndrome (CTS) develops initially, let’s explore why and how it can return after surgery.
What Causes Recurrent Carpal Tunnel Syndrome?
Even after successful initial treatment, carpal tunnel syndrome can be persistent. One primary cause is incomplete decompression during the surgery, which leaves residual pressure on the median nerve. Approximately 20% of patients experience recurrent symptoms post-surgery for this reason.
Scar tissue formation is another significant factor, as it can develop around the median nerve following surgery, leading to renewed pressure and symptoms.
Persistent Symptoms Post-Surgery
Some patients continue experiencing numbness, tingling, or pain after surgery, particularly if the median nerve was damaged before the procedure. Lingering symptoms commonly persist for several weeks post-operation.
Weakness in the hand or wrist is also a potential issue, often developing due to pain and the need to protect the surgical area. Moreover, post-surgical complications such as nerve injury or excessive scar tissue can lead to ongoing symptoms and may require further medical intervention.
It’s important to monitor for warning signs post-surgery, such as severe pain, persistent numbness, prolonged swelling around the site, or lack of symptom improvement.
Factors Contributing to Recurrence
Several factors can contribute to the recurrence of carpal tunnel syndrome:
- Medical conditions like diabetes, hypertension, and rheumatoid arthritis increase the likelihood of median nerve damage and subsequent recurrence.
- Wrist fractures can predispose individuals to recurrent symptoms.
- Anatomical differences can also play a role in the return of symptoms.
Factors relating to the initial surgery may also contribute. Incomplete release of the tendon during the original intervention can result in ongoing pressure on the median nerve. Additionally, swelling at the surgical site and inflammation of the tendons in the wrist area can lead to symptom recurrence.
Addressing these underlying issues is often key to effective management and preventing further complications.
The Role of Scar Tissue
Scar tissue formation is a significant factor in carpal tunnel syndrome recurrence. Following surgery, scar tissue may form around the median nerve, compressing it and leading to renewed symptoms.
Understanding this mechanism is helpful for both preventing and managing recurrent cases, especially in cases where scar tissue is the culprit.
How Long After Surgery Can Recurrence Happen?
The postoperative timeline for the recurrence of carpal tunnel syndrome widely varies. Current estimates suggest about one-third of patients experience symptom recurrence at some point in time. However, this can happen anywhere from 1 month to 5 years following surgery. The interval between initial and revision surgeries demonstrates this variability, ranging from 1 to 312 months in documented cases. This wide window underscores the importance of long-term monitoring.
Diagnostic Methods for Recurrent Carpal Tunnel Syndrome
Diagnosing recurrent carpal tunnel syndrome requires precise evaluation. Nerve conduction studies (NCS) are considered the gold standard for diagnosing CTS, as they provide measurable insights into the median nerve’s health. The sensitivity of these studies can be enhanced by comparing the median nerve to the ulnar nerve.
Ultrasound imaging can also be utilized to assess the median nerve’s cross-sectional area, helping to confirm the diagnosis of CTS. Electromyography (EMG) helps identify axonal damage by detecting specific spontaneous activities in the muscles innervated by the median nerve.
These diagnostic tools can accurately confirm recurrence and determine appropriate treatment strategies.
Treatment Options for Recurrent Carpal Tunnel Syndrome
Patients with recurrent symptoms have multiple treatment approaches available, both non-surgical and surgical. Non-surgical interventions can be effective for managing symptoms, but surgical treatments might be necessary for more severe cases.
Non-Surgical Interventions
Non-surgical interventions include wrist splinting, corticosteroid injections, and physical therapy.
Wrist splinting provides symptom relief by immobilizing the wrist and limiting aggravating movements. Corticosteroid injections help reduce inflammation and pain, while physical therapy focuses on strengthening and stretching exercises to improve wrist function. Consistently following prescribed physical therapy exercises is essential for optimal recovery.
Surgical Treatment
For patients whose symptoms persist despite non-surgical interventions, surgical treatment may be recommended.
Revision surgery is sometimes necessary to address issues related to scar tissue or incomplete decompression. Advanced microsurgical techniques, including the use of muscle flaps or synthetic nerve wraps, can help improve surgical success rates by providing better nerve protection and minimizing scar tissue formation.
Prevention Strategies
Preventing carpal tunnel syndrome recurrence involves both lifestyle adjustments and proactive measures.
Using ergonomic tools like wrist rests and split keyboards can reduce pressure on the median nerve during daily activities. Regular breaks from repetitive hand and wrist movements, ideally for 10 to 15 minutes every hour, are also beneficial. Gentle wrist stretches during breaks can prevent stiffness and maintain flexibility. Wrist splints can provide additional support.
Early consultation and habit changes can improve the chances of avoiding recurrence. When consistently practiced, these measures help to resolve symptoms by alleviating wrist pain and preventing excessive strain on the wrists.
Seeking Professional Guidance
Professional medical evaluation is key to accurate diagnosis and personalized treatment plans, especially in severe or recurrent cases. Early medical intervention can help prevent further nerve damage in cases of recurrent carpal tunnel syndrome.
Your orthopedic surgeon can offer specific recommendations for activity modification and prevention strategies tailored to your individual needs and risk factors.
Summary
Recurrence of carpal tunnel syndrome is a complex issue influenced by multiple factors such as incomplete decompression, scar tissue formation, and underlying medical conditions. Understanding these causes and the available treatment options is key to managing and preventing recurrence.
By taking proactive measures, seeking professional guidance, and exploring both non-surgical and surgical treatments, patients can effectively manage recurrent carpal tunnel syndrome. Staying informed and vigilant can help ensure a better quality of life and long-term relief from symptoms.
Frequently Asked Questions
Can carpal tunnel syndrome come back after surgery?
Yes, carpal tunnel syndrome can recur after surgery, often due to incomplete decompression, scar tissue formation, or underlying medical conditions. It’s important to monitor symptoms and consult your doctor if they arise again.
What are the common symptoms that persist after carpal tunnel surgery?
Patients may experience numbness, tingling, pain, and weakness in the hand or wrist. These issues can vary in intensity and may require further evaluation or treatment.
How long after surgery can carpal tunnel syndrome recur?
Carpal tunnel syndrome can recur anywhere from 1 month to 5 years after surgery, depending on various factors. It’s essential to monitor symptoms and consult your doctor if they return.
What non-surgical treatments are available for recurrent carpal tunnel syndrome?
For recurrent carpal tunnel syndrome, effective non-surgical treatments include wrist splinting, corticosteroid injections, and physical therapy. These approaches can help alleviate symptoms and improve function.
How can I prevent the recurrence of carpal tunnel syndrome?
Prevention focuses on ergonomic modifications (wrist rests and split keyboards), activity breaks for 10-15 minutes every hour, and gentle wrist stretches. Early consultation with your doctor for personalized modifications offers the best protection against recurrence.