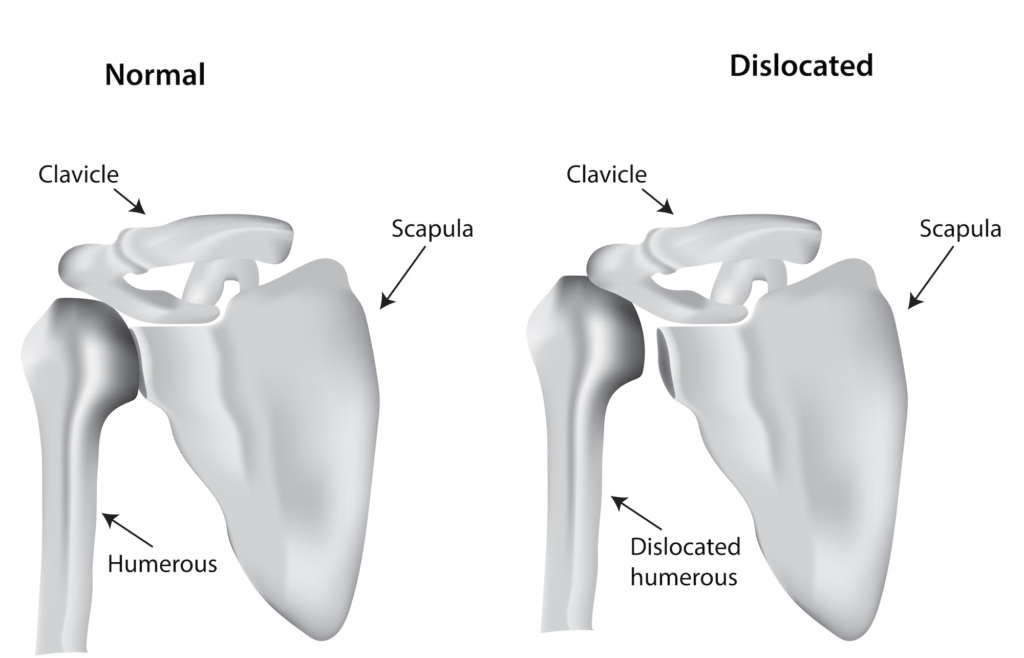
Shoulder instability occurs when the two components which make up the shoulder joint dislocate or experience a small amount of movement that prevents the shoulder from functioning normally.
In a healthy shoulder, the ball at the top of the humerus (upper arm bone) is held tightly against a concave surface on the scapula (shoulder blade) called the glenoid socket by a group of muscles called the rotator cuff. In order for the shoulder to function well and remain pain-free, the joint needs to remain stable at all times. When two pieces of the shoulder joint are no longer fitting nicely together, we call that shoulder instability.
Two kinds of shoulder instability
Trauma related Instability
This is when a traumatic event results in the dislocation of the shoulder. Usually, in this scenario, a patient would be seen in the emergency room, and the ER realigns the shoulder joint to get the ball back into the socket. But often, after one dislocation, the shoulder becomes prone to further dislocations.
Multi-directional Instability
For some patients, the reason the shoulder dislocates or is unstable is because they have an underlying soft tissue laxity problem. We call this type of shoulder problem multi-directional instability. These patients have shoulder instability without ever having had a traumatic injury.
Often, minor bumps that wouldn’t phase a healthy shoulder joint lead to instability and pain. The soft tissue is unnaturally relaxed and isn’t constraining the joint and holding it in place as it’s supposed to.
How do you check for shoulder instability?
I can usually determine if a patient is suffering from shoulder instability and what is causing it by taking a thorough medical history and examination.
Additionally, I also use MRI and X-ray, and CT imaging to evaluate the soft tissue or bony injuries and to confirm what the medical history is pointing to.
How do you treat traumatic shoulder instability?
When you dislocate your shoulder through a traumatic injury, changes occur in the anatomy of your shoulder, which makes it less stable and more likely to dislocate again.
One change that can occur is called a Bankart lesion, which happens when a shoulder dislocates anteriorly.
With a Bankart lesion, the labrum tears. The labrum is a special rim of cartilage that goes around the edge of the glenoid socket to deepen the joint space and hold the ball in place. Think about a golf ball resting on a golf tee; it’s not very stable.
When the labrum tears, it creates instability and allows the humeral head to slip out of place again. This is known as an anterior inferior(front) labral tear in the shoulder.
Another injury is the Hill-Sachs lesion. This occurs when the head of the humerus (upper arm) slips out of the socket and is compressed against the socket’s rim, causing an impaction fracture. The break creates a dent in the head of the humerus and leads to debilitating pain, and increases the chances for repeat dislocation.
For treatment options, I take into account the patient’s clinical presentation, their hobbies, if they are an athlete, whether they do hard physical labor or are sedentary.
Non-surgical options
Some patients can be treated with a non-operative approach. This would include physical therapy, immobilization, and anti-inflammatory medications.
Physical therapy can strengthen the muscles around the shoulder to help create more stability and prevent the shoulder from dislocating.
Many patients who are younger, especially those in their late teens and twenties, and who are still very active, are often not satisfied with conservative management. They tend to have a higher rate of re-dislocation because of their activity level and therefore benefit from surgery.
Surgical Options
Through surgery, we can repair the labral rim so that soft tissue constraints are in place to enable long-term future stability.
Another less common surgical option is called the Latarjet procedure. This technique is designed to augment or build up the existing glenoid with additional bone and is often used if a substantial portion of the shoulder socket has been worn away. It also uses what’s called the “sling effect” to add soft tissue constraint to the shoulder joint and prevent further dislocations.
When a patient receives the Lararjet procedure, the section of his scapula (shoulder blade bone), known as his coracoid process, is removed and transferred to the glenoid socket, along with the attached muscles and tendons. The additional bone and muscles act as a physical barrier that keeps the shoulder from dislocating again.
How do you treat multi-directional instability?
When a patient is showing signs of shoulder instability that did not result from trauma, our main treatment option is to engage the patient in intensive physical therapy. This type of healing takes time.
Occasionally a patient will fail to improve and will still be having pain after 6 to 12 months of intense conservative treatment. In that case, we can perform surgery to tighten the capsule in the front and back of the shoulder to take out some slack and stabilize the joint.
Patients sometimes want to have surgery right away, but it’s important that they attempt physical therapy for many months before we consider them a surgical candidate.